 |
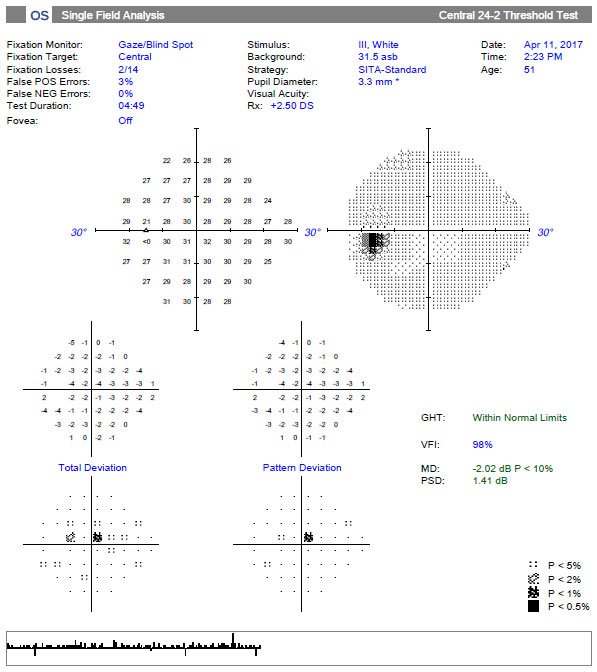
| Patient-centric communication could help improve eye care providers' understanding of visual impairment degree and visual field damage. Photo: Danica Marrelli, OD. Click image to enlarge. |
Good patient-physician communication is important for a variety of reasons such as treatment adherence and education, but a new study suggests that paying more careful attention to your patients may also serve as a useful adjunct to clinical testing when estimating glaucoma disease severity. “One specific challenge in communicating about glaucoma is that the treating physician doesn’t fully grasp what the patient sees, and the words they might use to describe these visual symptoms,” the researchers said. They noted that improving communication when discussing symptoms may help physicians better understand the patient’s degree of visual impairment and visual field (VF) damage.
In this cross-sectional study, the researchers imaged 170 adults (mean age: 64, 58% female) diagnosed with glaucoma (n=75) or suspicion of glaucoma (controls, n=95). They defined worse-eye VF damage on perimetric testing and retinal nerve fiber layer (RNFL) thickness on OCT. The patients rated their visual symptoms (frequency, severity) by answering questions from several published questionnaires on a scale of one (never/not at all) to four (very often/severe).
The researchers reported that among glaucoma patients, the mean median deviation of worse-eye VF damage was -19.3dB (range: -5.3dB to -34.7dB). The symptoms reported more commonly by glaucoma patients than suspects were better vision in one eye, blurry vision, glare, sensitivity to light, cloudy vision and little peripheral vision. The worse severity ratings for “little peripheral vision” explained the most variance in VF damage (43%), the researchers said.
They noted that the multivariable model (frequency of cloudy vision, severity of little peripheral vision, missing patches, one eye with better vision, vision worsening and sociodemographic factors) accounted for 62% of variance in VF damage. By comparison, the researchers reported that the multivariable model of worse-eye RNFL thickness and sociodemographic features explained 42% of VF damage variance, while the sociodemographic-only model explained 8% of VF damage variance.
The researchers concluded that the specific symptoms associated with degree of VF damage, cloudy vision, having little peripheral vision, missing patches, having better vision and vision worsening over time can provide useful additional information to judge glaucoma severity in the clinical setting. “These symptoms suggest specific terms that are likely to reflect glaucoma damage, which can be used when communicating with patients,” they explained, noting that missing patches may point to glaucomatous scotomas, cloudy vision can be understood “as the manifestation of contrast deficits which underlie glaucoma” and worsening vision may reflect VF severity because of a greater rate of worsening in severe disease. “Reporting worsening vision may also reflect the clinically-observed tendency of subjective vision to fluctuate more in advanced glaucoma, resulting in days of ‘worsening,’ though some corresponding days of ‘improvement’ would also be present,” the investigators wrote.
They suggest physicians strengthen their relationship with patients by showing that they understand the patient’s symptoms and the impact of the disease on their life. “Understanding what symptoms patients with severe glaucoma experience is uniquely important, as they may feel frustrated completing visual testing or lose faith in treatment due to their limited vision,” the researchers pointed out. “If physicians demonstrate an understanding of what specific symptoms are related to severe glaucoma and the impact on a patient’s vision, they may be able to better develop therapeutic alliances with patients,” they concluded.
Shah YS, Cheng M, Mihailovic A, et al. Patient reported symptoms demonstrating an association with severity of visual field damage in glaucoma. Ophthalmology. October 27, 2021. [Epub ahead of print]. |


