 |
|
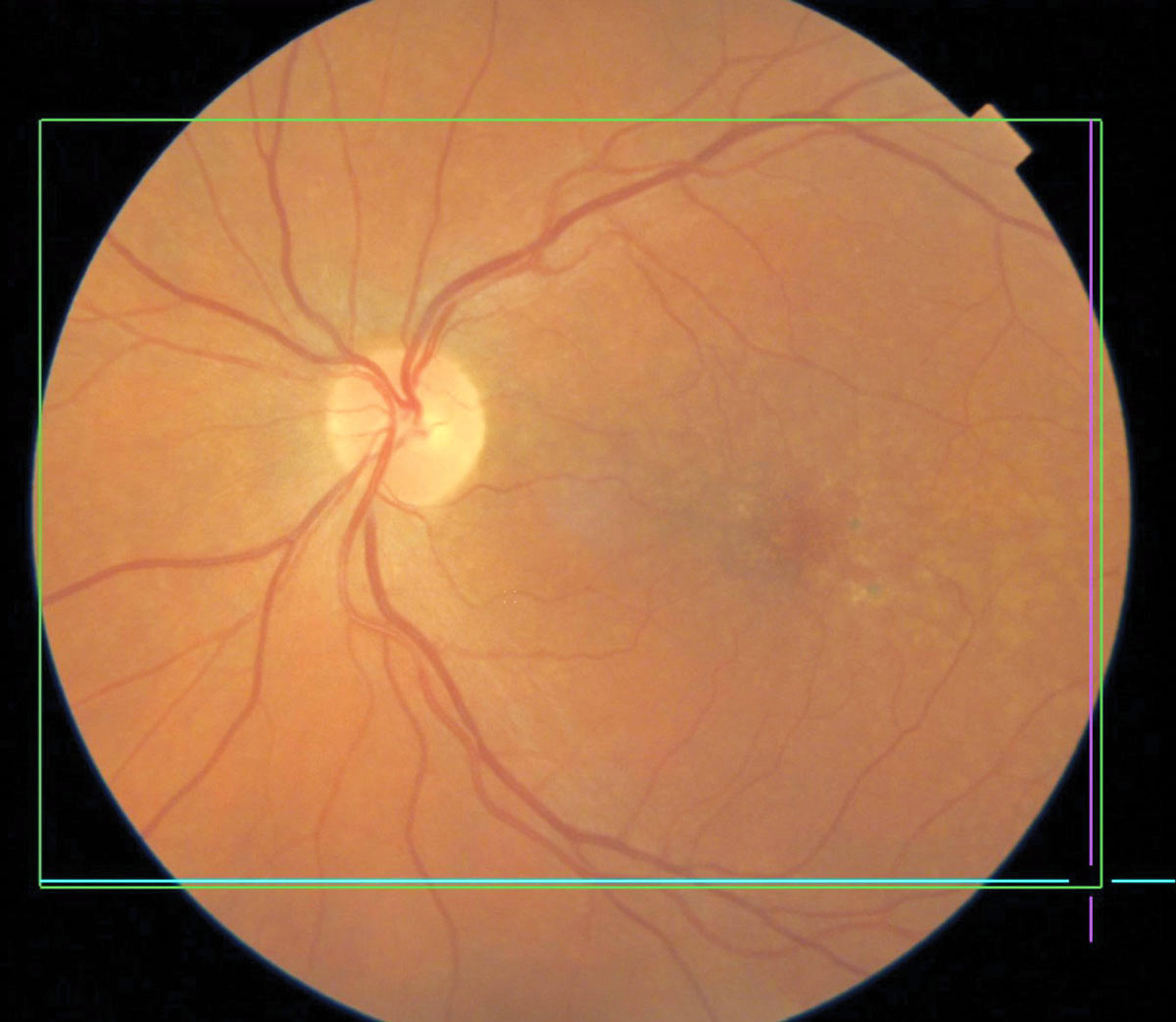
Patients with macular degeneration are at increased risk for dementia and Alzheimer's, study finds. Photo: Brian Chou, OD. Click image to enlarge. |
Editor’s Note: As part of our “Year in Review” retrospective, we’ve selected the top 30 news stories of the year and are re-sharing them as we close out 2022. Follow along as we count down to number 1!
This story was originally published on November 16, 2022.
No. 7 biggest news story of 2022:
With age-related macular degeneration (AMD) sharing several clinical and pathological features as Alzheimer’s disease (AD), one new study has sought to clarify epidemiological reports on the association between the two. Inconsistencies between AMD and subsequent dementia are present, thus warranting a new look.
The researchers conducted a meta-analysis of eight studies published between the years 2000 and 2021. Pooled hazard ratios of dementia or Alzheimer’s were estimated using a random-effects model. A total of 8,223,581 participants were included, with macular degeneration significantly associated with subsequent dementia. Even more specifically, the association was more prominent in cases of dry rather than wet AMD. Patients with AMD were found to have a 1.22-fold risk of dementia development and 1.21-fold Alzheimer’s risk compared to patients without macular degeneration.
The researchers offer a theory as to why they found a stronger association with dry AMD rather than the wet form with either cognitive condition. Angiogenesis is involved in amyloid-beta peptide deposition, a clinical marker of AD. Since angiogenesis may be involved in neurodegeneration, interventions that either directly or indirectly inhibit it may provide some beneficial effects against amyloid plaque development—a hallmark of AD—or other disease pathways. Increased levels of VEGF in cerebrospinal fluid and blood have been associated with AD’s clinical severity, and subsequently, intravitreal injections of anti-VEGF agents for those with wet AMD would likely result in a lesser association.
As for the more general association between AMD and dementia, multiple hypotheses exist. One proposes that the amyloid-beta plaques found in AD, when seen in drusen, may lead to progressive AMD through means of oxidative stress, uncontrolled inflammation and imbalanced angiogenesis. Similarly, both conditions display upregulation of inflammatory responses, displayed through high concentrations of complement factors in both patient subsets. AD patients display an elevated rate of a particular complement factor and an AMD-associated allele, potentially making this a risk factor for AMD patients to develop Alzheimer’s.
The authors focus on what clinicians can do for these high-risk patients. One option may be the Mini-Cog test, validated for patients with AMD in a prior study, to help aid early dementia or Alzheimer’s diagnosis. Following this logic, the authors propose that “routine cognitive assessment for high-risk patients may be warranted for the early recognition and management of dementia or AD.”
They also advocate for more action to disseminate this issue to the population. As they note in their AJO paper on the study, “given that researchers have identified certain retinal abnormalities as potential biomarkers for AD diagnosis and progression with advances in retinal imaging, clinicians should raise awareness of AD-related OCT biomarkers in patients with AMD.”
Tsai HR, Lo RY, Liang KH, et al. Risk of subsequent dementia or Alzheimer’s disease among patients with age-related macular degeneration: A systematic review and meta-analysis. Am J Ophthalmol. 2022. [Epub ahead of print]. |


