 |
|
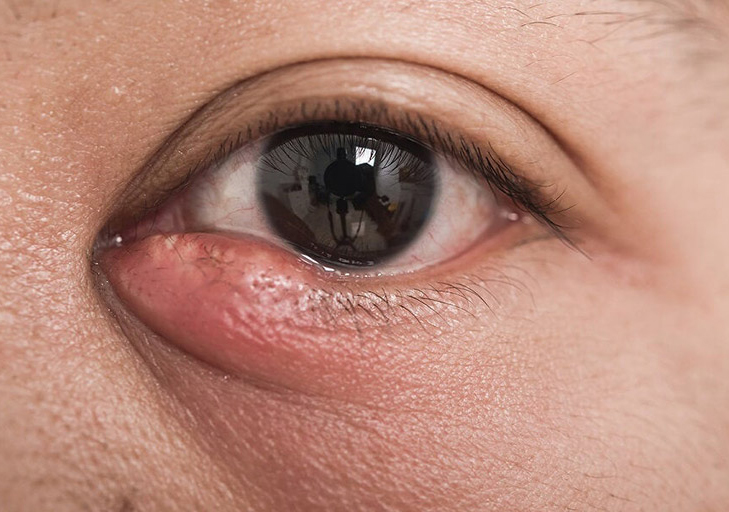
Postmenopausal women with obstruction of the nasolacrimal duct exhibit significant morphological changes in the meibomian gland. Photo: Abraham Gomez, MD/Arte Facial. Click image to enlarge. |
Primary acquired nasolacrimal duct obstruction (PANDO) is frequently encountered in perimenopausal women, causing tear flow stagnation and resulting in a variety of ocular discomfort symptoms. However, little is known about the alterations in the meibomian gland (MG) in these women. A recent study investigated the MG and ocular surface and found that affected women exhibit significant morphological changes.
This study included 60 eyes of 60 postmenopausal women with PANDO and 30 eyes of 30 postmenopausal women without PANDO. The affected subjects were subdivided into incomplete and complete PANDO categories based on the degree of nasolacrimal duct obstruction. Symptoms were evaluated using the ocular surface disease index questionnaire, and the MG and ocular surface were assessed using the Keratograph 5M. Other ophthalmologic examinations included tear breakup time, corneal fluorescein staining, MG expression and Schirmer I test.
Severe MG loss and ocular surface discomfort were found in patients with duct obstruction. Postmenopausal women with the condition also had a higher noninvasive tear meniscus height, which is associated with the degree of nasolacrimal duct obstruction. Because of this, noninvasive tear meniscus height may serve as a valuable objective index for assessing the severity of lacrimal duct obstruction in clinical settings, according to the study authors.
“In contrast, postmenopausal women with PANDO had lower corneal fluorescein staining and MG distortion of the upper eyelid scores, which were inversely correlated with the degree of nasolacrimal duct obstruction,” they wrote in their paper. “Hence, PANDO protects the integrity of the corneal epithelium and prevents MG distortion, which may be related to the alleviation of tear hyperosmolarity in postmenopausal women.”
After controlling for sex and age—the greatest risk factors for MG dysfunction—the authors found that the loss ratio of the upper eyelid was significantly higher in patients with incomplete obstruction than the control group, and the loss ratio of the lower eyelid was significantly higher in patients with incomplete closure than in patients with complete blockage. “Thus, MG loss appears to be more prominent in patients with incomplete PANDO,” the authors noted.
MG loss did not bear a positive relation with the degree of nasolacrimal duct obstruction. “However, the MG orifices, secretion expressibility and meibum quality were not altered significantly in PANDO,” they wrote. “Therefore, we postulated that the classical ‘ductal centric’ hypothesis was not applicable to the pathomechanism underlying MG loss aggravated by PANDO. More attention should be paid to MG loss in postmenopausal women with incomplete PANDO, as it is crucial for identifying MG impairments in patients with PANDO.”
Jin H, Zhang H. Changes in meibomian glands in postmenopausal women with primary acquired nasolacrimal duct obstruction: a prospective study. BMC Ophthalmol. February 1, 2023. [Epub ahead of print]. |


