 |
|
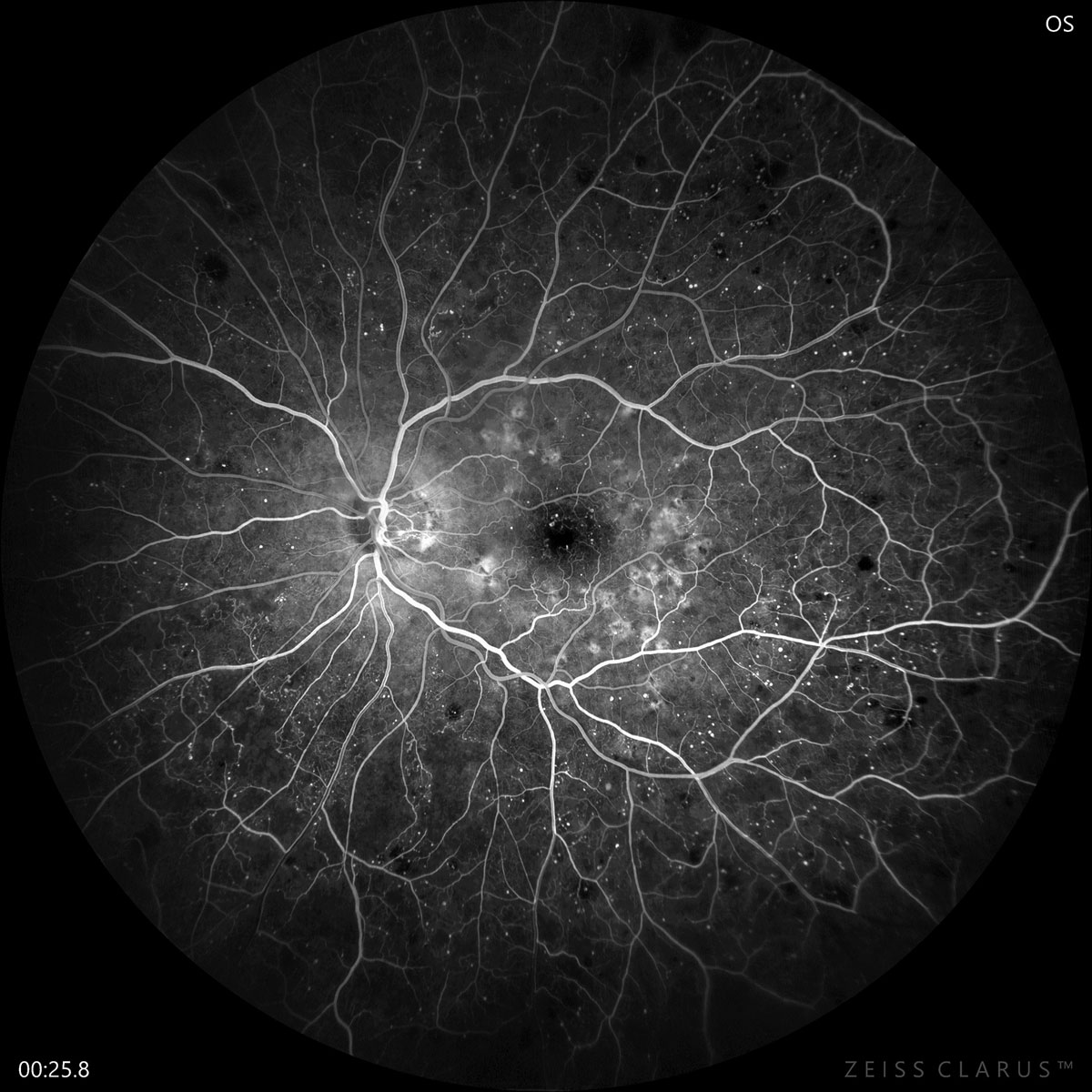
Compared with previous research, this study identified lower rates of prevalence, incidence and progression of DR among type 2 diabetes patients. Photo: Jay Haynie, OD. Click image to enlarge. |
An analysis on patients with type 2 diabetes conducted in Denmark recently evaluated the prevalence and incidence of diabetic retinopathy (DR), one of the most common complications of the disease. The researchers identified the use of insulin and duration of diabetes to be the two most important predictors of DR development.
Data was retrieved from the Danish Registry of Diabetic Retinopathy, which included 153,238 patients (56.4% male) with type 2 diabetes who had attended at least one DR screening between 2013 and 2018. DR was classified as levels zero to four from least to most severe.
The mean age of patients in the study was 66.9 years, and the mean duration of diabetes was 5.3 years. The prevalence of DR was 8.8%, the five-year incidence of DR was 3.8%, the percentage of patients with at least a two-step progression of DR was 0.7% and the percentage of patients who progressed to proliferative DR (PDR) was 0.2%.
The leading factors associated with DR development or progression were disease duration (hazard ratio [HR]: 1.98) and insulin use (HR: 1.88). Type 2 diabetes patients using insulin were 2.3-times more likely to have DR and at a 1.9- to 2.4-times higher risk of developing the condition or experiencing progression. Younger age was also identified as an associated factor (HR: 0.88). Alternately, the use of cholesterol-lowering medicine appeared to be a protective factor, resulting in a 30% reduced risk of developing PDR.
Interestingly, the researchers also observed that the three-year incidence rate of PDR decreased between 2013 and 2015 from 1.22 to 0.45 events per 1,000 person-years.
“While there were not clinically relevant differences between the years according to most parameters, there were statistically significant and clinically relevant changes from 2013 to 2018 with respect to lower use of insulin (20.6% to 12.8%), blood pressure-lowering therapy (80.4% to 74.0%) and cholesterol-lowering therapy (79.9% to 73.4%),” the researchers noted in their paper. Hospital-based DR screening also decreased from 27.4% in 2013 to 7.1% in 2018.
This analysis—part of the Ocular and Systemic Complications in DR Study (OASIS)—found a lower prevalence, incidence and progression of DR compared with prior studies that looked at data on fewer patients. The researchers suggest that this may in part be due to the advancement of therapy and risk factor reduction for type 2 diabetes in recent years.
“Upcoming studies of the OASIS project will be able to address long-term outcomes of DR and how these are influenced by systemic diseases and intervention,” the researchers concluded.
Grauslund J, Pedersen FN, Andersen, N, et al. Presence and development of diabetic retinopathy in 153,238 patients with type 2 diabetes in the Danish Registry of Diabetic Retinopathy. Acta Ophthalmol. October 3, 2022. [Epub ahead of print]. |


