 |
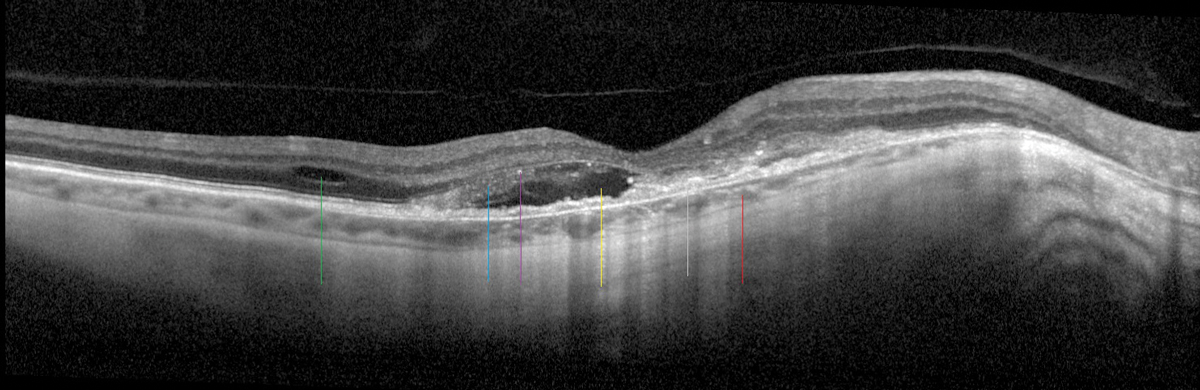
| A highly myopic patient with a tessellated and thin choroid (red line), RPE disruption (gray line), SRF (yellow line), IRF (green line), edematous photoreceptors (blue line) with early tubulation and hyperreflective material (purple line) are all consistent with myopic CNV. Photo: Sara Weidmayer, OD. Click image to enlarge. |
Researchers recently conducted a pooled analysis to determine the prevalence, risk factors and predictors of myopic macular degeneration (MMD) among Asian patients, who tend to have higher myopia rates. Patients with high myopia are at an especially increased risk for MMD, with a prevalence between 13.3% and 72.7%. The team discovered several risk factors for MMD, but spherical equivalent (SE) was the most reliable predictor.
A total of 21,264 participants from seven cross-sectional studies were included in the analysis. Of these, 19,885 participants were from population-based studies and 1,379 were highly myopic. The researchers used fundus photographs to grade MMD and defined the condition as the presence of diffuse choroidal atrophy and patchy chorioretinal or macular atrophy with or without a “plus” lesion (lacquer crack, choroidal neovascularization, Fuchs’ spot).
The prevalence of MMD based on location was as follows: 0.4% in rural India, 0.5% in Beijing, 1.5% in Russia and 5.2% in Singapore. The investigators found that older age, female gender, lower education level, greater myopia severity and longer axial length (AL) were all risk factors for MMD. Myopic refractive error was noted to be the strongest single predictor of MMD, with an AUC of 0.92. AUC values for the other predictors in decreasing order were AL: 0.87, age: 0.67, education: 0.55 and gender: 0.53.
“The addition of age, education and gender to the prediction of myopia on MMD only improved the AUC marginally from 0.92 to 0.94,” the researchers wrote. “A simple measure of SE alone is cost-effective and easy to implement in most settings with an inexpensive apparatus, compared with AL measurement with specialized equipment that is often lacking in primary care settings. For efficient risk profiling of individuals, those with greater myopic SE can be identified as individuals at higher risk of MMD. However, this would not be applicable for individuals with altered SE, such as those who have undergone cataract or refractive surgeries.”
Take extra precautions with your myopia patients, particularly those with severe levels of myopia or additional risk factors, when monitoring for MMD and preventing irreversible visual outcomes.
Wong YL, Zhu X, Tham YC, et al. Prevalence and predictors of myopic macular degeneration among Asian adults: pooled analysis from the Asian Eye Epidemiology Consortium. Br J Ophthalmol. 2021;105:1140-8. |


