 |
|
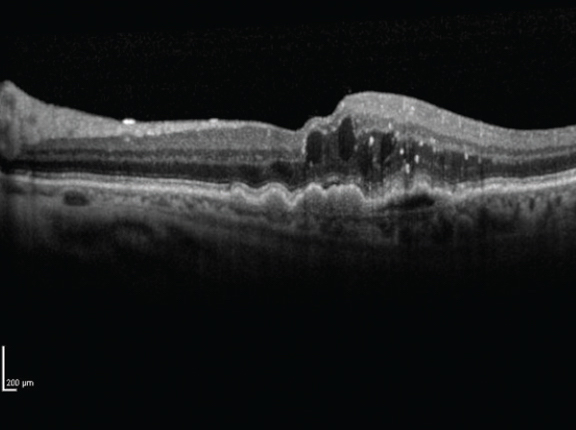
Wet AMD patients treated with new drug OPT-302 had better visual gains than the sham in this Phase II trial (14.2 vs. 10.8 letters). Click image to enlarge. |
A Phase IIB trial just published in the journal Ophthalmology describes promising results for a new approach to neovascularization. Sponsored by the drug’s developer, Opthea, the trial’s safety and efficacy data gives new context on its potential outcomes and adverse events in wet AMD patients.
Specifically, patients were given intravitreal injections of either 0.5mg or 2.0mg of OPT-302 or a sham alongside 0.5mg of the anti-VEGF-A inhibitor ranibizumab. A total of 366 patients without previous treatment for wet AMD were included from 109 sites across Europe, Israel and the US. The injections were administered four times a week for six weeks.
After the course of treatment, the researchers found visual acuity gain of the 2.0mg group to be superior to the sham, with a mean gain of 14.2 ±11.6 letters (vs. 10.8 ±11.5 for sham), while the 0.5mg group was not found to differ significantly from the sham. Even further, the percentage of patients who gained 10 or more letters was greater than in the sham group, at rates of 70.0% and 57.8%, respectively. This was coupled by a reduced likelihood of the high-dose group to experience loss of 10 or more letters, with rates of 0.8% vs. 6.0%.
Additional best-corrected visual acuity outcomes were favored in the 2.0mg group. Structural, anatomical outcomes favored both dosage groups, and development of at least one serious adverse event happened at similar rates throughout all groups, with 8.3% incidence in the sham group, 13.3% in the lower dose and 5.6% in the higher dose.
The authors of the study point out that while differences are present for eligibility criteria, dosing and follow-up between studies, the vision gain observed in this trial compares to that seen with 12-month registration studies for anti-VEGF-A intravitreal therapies. The observed gain here was of +14.2 letters—though with a fairly high standard deviation of 11.6—while the anti-VEGF-A therapies saw gains of +6.1 and +10.9.
Suppression of VEGF-A results in upregulation of VEGF-C and VEGF-D, an effect that may limit the efficacy of selective VEGF-A inhibition., the authors speculate in their paper. ”Compensatory upregulation of VEGF-C and -D may explain why at least 45% of patients show some degree of resistance to VEGF-A inhibitors, failing to improve, maintain or achieve optimal vision responses.” they propose. Coadministration of a therapy that suppresses VEGF-C and -D “therefore has the potential to improve both short-term and long-term outcomes.”
Looking at this finding, the authors of the study emphasize that, “notwithstanding the clinical relevance of reduced dosing and reduced cost, many patients’ key aim is to preserve or improve their vision, and a drug that has the potential to provide the best visual outcomes would have considerable clinical utility.”
A future treatment protocol that combines OPT-302 with an anti-VEGF-A agent may offer advantages over current approaches, especially when considering that anatomical improvements occurred in both OPT-302 groups compared to the sham, specifically by means of greater reduced central subfield thickness seen in both cohorts along with better retinal drying. While the anatomic improvements seen in the low-dose group did not translate to better vision, the authors explain that anatomic improvement can precede vision gain and speculate differences could occur over time.
Despite this inconsistency, when looking at the high dose group the authors do believe that “VEGF-C and -D inhibition with 2.0mg OPT-302 in combination with VEGF-A blockade achieves superior vision gains compared to the current standard of care for nAMD, with anatomic benefits and a favorable safety profile.”
Jackson TL, Slakter J, Buyse M, et al. A randomized controlled trial of OPT-302, a VEGF-C/D inhibitor for neovascular age-related macular degeneration. Ophthalmology. 2023. [Epub ahead of print]. |


