 |
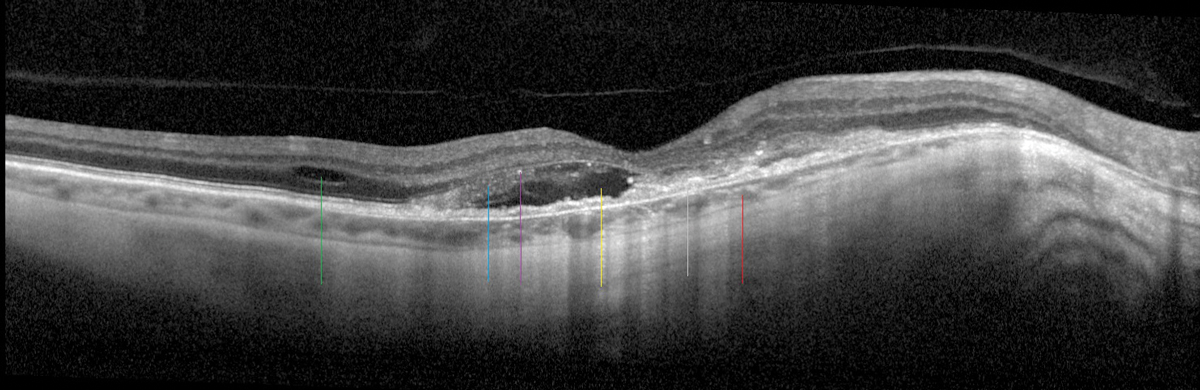
| Using OCT-A regularly on patients with myopic CNV on anti-VEGF therapy can help monitor treatment response. Photo: Sara Weidmayer, OD. Click image to enlarge. |
More clinicians as of recent have used optical coherence tomography angiography (OCT-A) to detect myopic choroidal neovascularization (CNV), as it’s considered to be a promising tool for monitoring disease progression. Previous studies have shown associations with lesion size after anti-VEGF treatment in patients with myopic CNV. In this latest study, researchers aimed to identify baseline morphological predictors of lesion shrinkage in eyes with myopic CNV treated with anti-VEGF using OCT-A.
Forty-six eyes (41 patients) with active myopic CNV receiving anti-VEGF treatment were included. OCT-A was performed at baseline and one year after treatment. Eyes were classified as “high-shrinkage” or “low-shrinkage” according to the median relative change in lesion area. Baseline quantitative morphological features associated with myopic CNV shrinkage were identified in univariate and multivariate analyses, and the authors calculated the endpoint density as the number of endpoints in open-ended vessels per unit vessel length, which reflected the activity of sprouting capillaries.
The myopic CNV area was significantly smaller after one year with a median relative change of -16.5%. The relative change in myopic CNV area was -48.3% in high-shrinkage eyes (n=23) and -5.2% in low-shrinkage eyes (n=23). High-shrinkage eyes had a smaller myopic CNV area, shorter total vessel length and higher endpoint density. Multivariate analysis showed significant associations of high shrinkage with endpoint density and previous anti-VEGF treatment.
The authors found that the endpoint density was a consistently significant factor in myopic CNV shrinkage in both univariate and multivariate regression models, which suggests higher endpoint density contributes to shrinkage of the lesion after antiangiogenic therapy.
Since not all eyes were treatment-naive, the role of previous anti-VEGF treatment in myopic CNV shrinkage was also evaluated. “Multivariate regression models showed that myopic CNV shrinkage was more likely in treatment-naive eyes than in eyes with a history of anti-VEGF therapy, which suggests that myopic CNV may become resistant or refractory to anti-VEGF agents,” the authors explained. “A possible explanation for this finding is that anti-VEGF agents can prune newly formed capillaries but have no effect on larger vessels covered by pericytes and smooth muscle cells.”
In conclusion, OCT-A is shown to be a promising imaging technique for assessment and prediction of the response to anti-VEGF therapy in patients with myopic CNV, and the baseline endpoint density of myopic CNV was found to be a useful morphological feature in predicting lesion shrinkage.
Liu J, Song S, Yu X, et al. Predicting lesion shrinkage in eyes with myopic choroidal neovascularization from features on optical coherence tomography angiography. Retina. May 11, 2022. [Epub ahead of print]. |


