 |
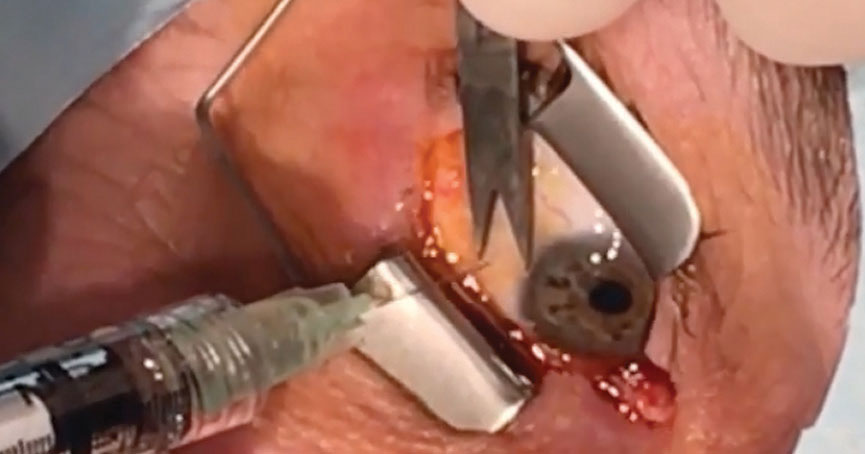
| Researchers highlight the phenomenon that while preoperative injections may increase risk, postoperative injections seem to have quite the opposite effect, especially in quantities of seven or more. Photo: Leonid Skorin Jr., DO, OD. Click photo to enlarge. |
Research has speculated that intravitreal injections (IVIs) may increase intraocular pressure (IOP) and counteract glaucoma surgery outcomes in patients who have undergone both forms of treatment. To examine whether postoperative IVIs are associated with a higher failure rate for trabeculectomy and glaucoma drainage device (GDD) surgeries, researchers reviewed the charts of 133 glaucoma patients (133 eyes) who underwent one of the two procedures and received at least one IVI preoperatively. All patients underwent either GDD or trabeculectomy at Massachusetts Eye and Ear between 2005 and 2020, with 94 undergoing IVIs after surgery.
Overall, the researchers reported similar levels of IOP, medication burden and visual acuity outcomes between the two groups, with the exception of two specific time points: at six weeks post-op, when the mean IOP was lower in patients with postoperative IVIs (15.2mm Hg and 18.8mm Hg, respectively), and three years after the glaucoma procedure, when IOP decreased from 32.5mm Hg to 15.5mm Hg for the group with postoperative IVIs and from 32.9mm Hg to 12.6mm Hg for the group without. The researchers suggest this is because the effects of postoperative IVIs may require cumulative injections.
The two groups had comparable success rates; however, when stratified by the number of IVIs, the group with seven or more postoperative injections had significantly higher success rates than those with zero to six. This finding suggests that IOP-reducing benefits from IVIs may only be observed after multiple IVIs.
“Each additional postoperative IVI resulted in a 7.2% decrease in the hazard of failure to achieve our above success criteria,” the researchers wrote in their study. “With regard to late complications, the group with postoperative IVIs had a higher incidence of vitreous hemorrhage than the group without postoperative IVIs (18.5% vs. 3.2%). This is likely confounded by the fact that patients with vitreous hemorrhage would require IVIs with anti-VEGF medications.”
The researchers noted, “It is interesting that having multiple preoperative IVIs may increase the risk of glaucoma surgery, while having multiple postoperative IVIs may decrease the risk of failing to achieve successful IOP reduction.” More studies may help to explore the benefit of multiple postoperative IVIs on the outcomes of traditional glaucoma surgery.
Chang EK, Gupta S, Hall N. Effects of postoperative intravitreal injections (IVIs) on outcomes of traditional glaucoma surgery in patients with preoperative IVIs. Ophthalmology. August 30, 2021. [Epub ahead of print]. |


