 |
|
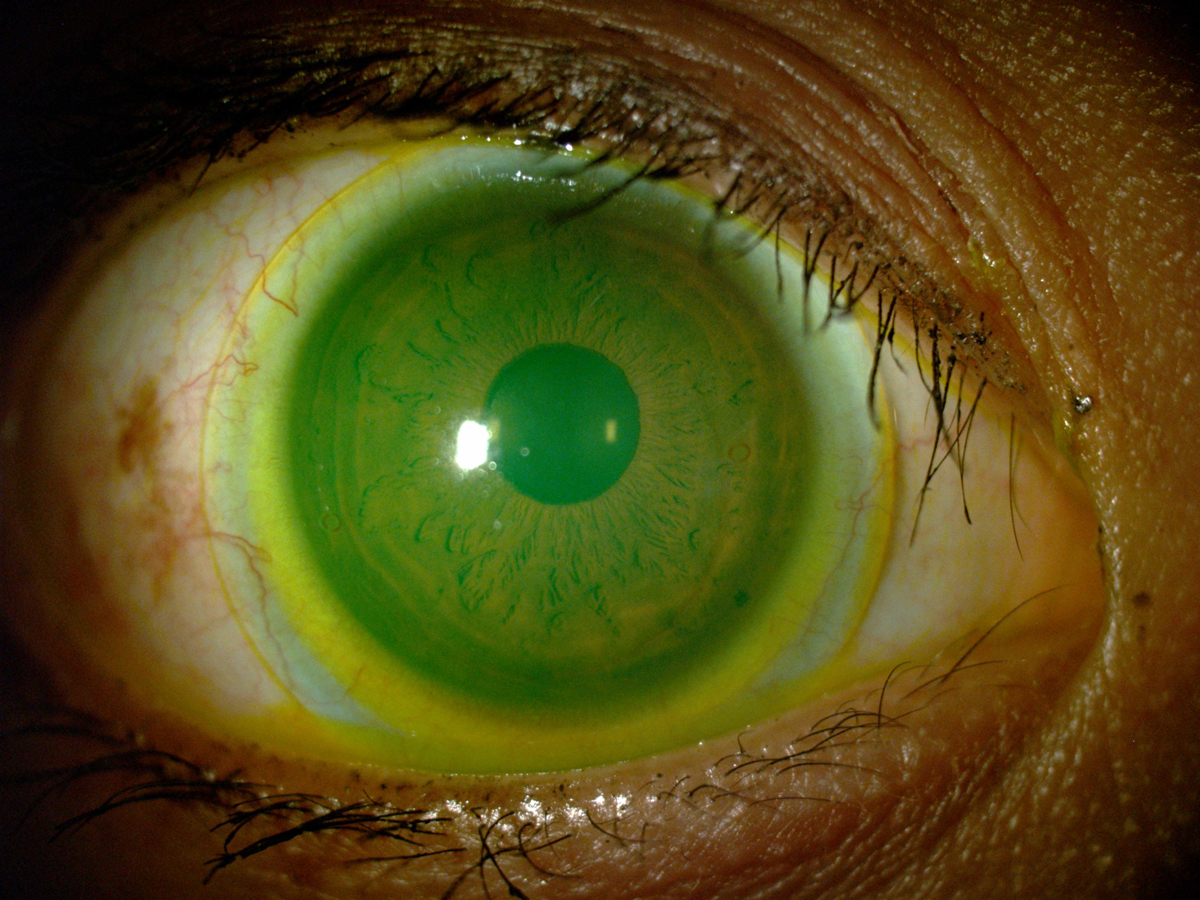
Practitioners now appear to prescribe nonspherical landing zone designs for scleral lenses more frequently than originally thought. Click image to enlarge. |
Updated information about scleral lens prescription and management encompassing all practice types is needed to determine the extent to which research and industry advancements have affected clinical practice. In 2020, the Scleral Lenses in Current Ophthalmic Practice Evaluation (SCOPE) study team conducted a survey-based study, following a similar 2015 investigation. This time, the researchers found that practitioners increasingly are prescribing sclerals with advanced landing zone designs, as well as recommending hydrogen peroxide-based disinfection systems and single-use vials of preservative-free saline for lens care and application.
An online survey was designed by the SCOPE study team and administered to eyecare practitioners attending a specialty contact lens meeting. There were 715 practitioners who responded to at least one item of interest (lens diameter, landing zone design, lens care recommendation and ancillary testing performed during routine follow-up examination) along with at least one item querying demographic information.
Most lenses prescribed (63%) were 16mm or more in diameter. Lenses with toric landing zones were the most frequently prescribed (48%), followed by spherical (40%), quadrant-specific (8%) and impression- or image-based designs (3%). Large standard deviations in the distribution of data for both lens diameter and design suggests that considerable differences remain for individual prescribing patterns. These differences may result from the practitioner’s preference or fitting philosophy.
Most participants (61%) recommended hydrogen peroxide products for lens care. Preservative-free saline in a single-use vial was most frequently recommended to fill the bowl of the lens before application.
Intraocular pressure was measured during lens evaluation by 45% of participants, and 38% of participants routinely measured corneal thickness.
“According to the current study, virtually all practitioners reported routinely assessing for corneal and conjunctival staining after lens removal; however, just over one-third of practitioners reported assessing corneal thickness, almost half reported measuring IOP and just over half of practitioners reported that they evert the upper eyelids to evaluate the superior tarsal conjunctiva during routine scleral lens evaluation,” the researchers wrote in their paper for Eye & Contact Lens. They found that this finding raised questions as to why routine evaluation of corneal thickness, intraocular pressure and the superior tarsal conjunctiva is not performed regularly by a higher percentage of practitioners.
Overall, the team believes that the information collected may allow clinicians to reflect on whether their scleral lens protocols represent the current standard of care for lens design, recommended care products and examination components of standard lens evaluations.
“As best practices within the scleral lens community continue to evolve, it may be helpful to reach a consensus on the essential components of lens evaluation and to regularly administer standardized assessment instruments of patient-reported outcomes, which could more effectively quantify benefits of specialty lens wear,” they concluded.
Schornack M, Nau C, Harthan J, et al. Current trends in scleral lens prescription, management and evaluation. Eye Contact Lens. November 10, 2022. [Epub ahead of print]. |


