 |
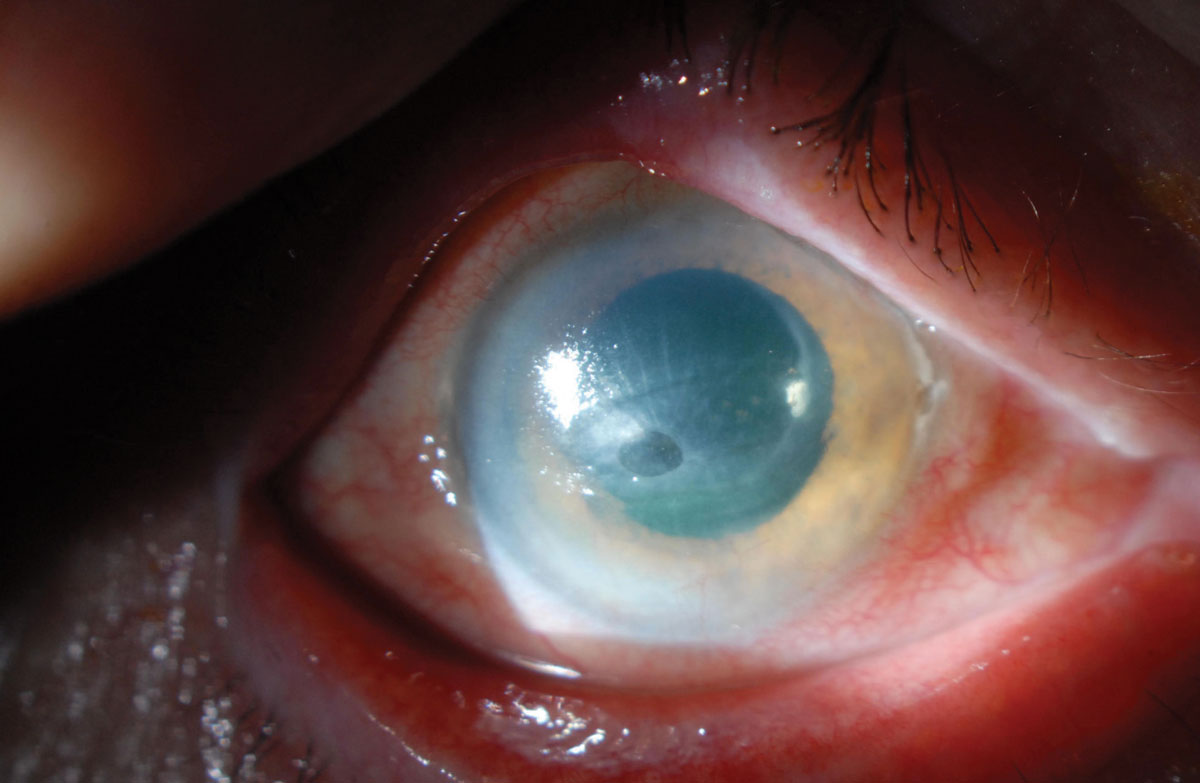
Patients with neuropathic pain may respond uniquely to different treatment options. Click image to enlarge. |
Ocular surface pain, especially when chronic, may have a neuropathic component in some patients involving dysfunction of the mechanisms at the peripheral or central nerves. Treatment efficacy may be hard to assess considering how such pain manifests in the ocular system; while physiological and neural processes are what signal the pain, complex non-neural mechanisms, including emotional and psychological factors, also affect the sensation and maintenance of pain. A team of researchers performed a study to more clearly determine the clinical responses to common treatment modalities in patients with neuropathic ocular surface pain.
The study included 101 patients with a clinical diagnosis of neuropathic pain who were seen at the University of Miami Oculofacial Pain Clinic between January 2015 and August 2021. Data from medical records including comorbid conditions and information on current or previous medication use or treatments was collected for each patient. The cohort was divided into the following three subcategories based on the type of pain each patient was experiencing:
Post-surgical: pain that developed after undergoing surgery (e.g., refractive or cataract)
Post-traumatic: pain that followed a non-surgical trauma such as chemotherapy, radiation or brain injury
Migraine-like: bilateral pain that started spontaneously and was accompanied by photophobia and, typically in this cohort, migraine or headache
Unilateral: pain that started spontaneously, did not follow surgery, was not typical for trigeminal neuralgia and had neuropathic qualities
There were various treatment modalities used among the study population. The researchers wrote, “The most common oral medications were α2δ ligands (48.5%), nonsteroidal anti-inflammatory drugs (31.7%) and serotonin-norepinephrine reuptake inhibitors (16.8%). Oral medications were commonly paired with topical therapy, such as autologous serum tears (20.8%) and/or a topical anti-inflammatory (e.g., topical steroid [19.8%], cyclosporine or lifitegrast [17.8%] or less commonly tacrolimus [8.9%]). Finally, a minority of patients received adjuvant therapies, including trigeminal nerve stimulation (TNS, 15.8%), steroid/anesthetic-based periocular nerve block (24.8%) and/or botulinum toxin injections (10.9%).”
The researchers made the following conclusions from their analysis of the recorded clinical responses from each treatment method:
At least one oral medication reduced pain to a mild degree or greater for most patients in the post-traumatic (81.2%), migraine-like (73%) and unilateral pain (72.7%) groups but in only 38.5% of the post-surgical pain patients.
Marked improvement from treatment with oral medications was most frequently found in migraine-like patients (21.6%) and to a lesser degree in the other groups (post-surgical 15.4%, post-traumatic 12.5%, unilateral 0%).
Topical medication subjectively improved pain in the post-traumatic (66.7%), migraine-like (78.6%) and unilateral (70%) groups more often than in the post-surgical group (43.7%). Marked improvement was also most common in migraine-like patients for this treatment (21.4%).
One or more adjuvants reduced pain to a mild degree or greater in the post-surgical (54.5%), post-traumatic (71.4%) and migraine-like (73%) groups but did so for 0% of patients in the unilateral group.
As is clear from the data, responses to a number of different treatment methods vary heavily between pain subgroups. The team concluded that migraine-like pain sufferers report the most frequent symptom improvement and that the most effective therapy for this population seemed to be a combination of oral (α2δ ligands) and adjuvant (TNS) therapies.
On the other hand, “The post-surgical group had the lowest overall response rate (40.7%) to the various therapies,” the researchers wrote. “This highlights the need for further studies to investigate other, more appropriate therapies to target the pain in this population. Furthermore, we found that the likelihood and degree of pain improvement increased with longer follow-up time and with the number of medications utilized, indicative of inter-individual variability that necessitated multiple trials of medications to find a combination that led to clinical improvement.”
The researchers concluded that although treatment responses vary by individual, trends can be observed among pain subgroups. Future studies will hopefully identify ways to pinpoint the location(s) of nervous system dysfunction to decrease reliance on a trial-and-error therapeutic approach.
Patel S, Mittal R, Felix ER, et al. Differential effects of treatment strategies in individuals with chronic ocular surface pain with a neuropathic component. Front Pharmacol. 2021;12:788524. |


