Myopia Literature ReviewFollow the links below to read other summaries in this series: |
Myopia is a growing epidemic, and optometrists are increasingly expected to mitigate it rather than just correct it. As the research is vast and more than any single OD could realistically follow, experts at the Brien Holden Vision Institute recently published a series of literature reviews (think DEWS II, but for myopia) to help clinicians better understand the disease, current research efforts and management options. Review of Optometry selected three key papers to summarize; all nine are available here.
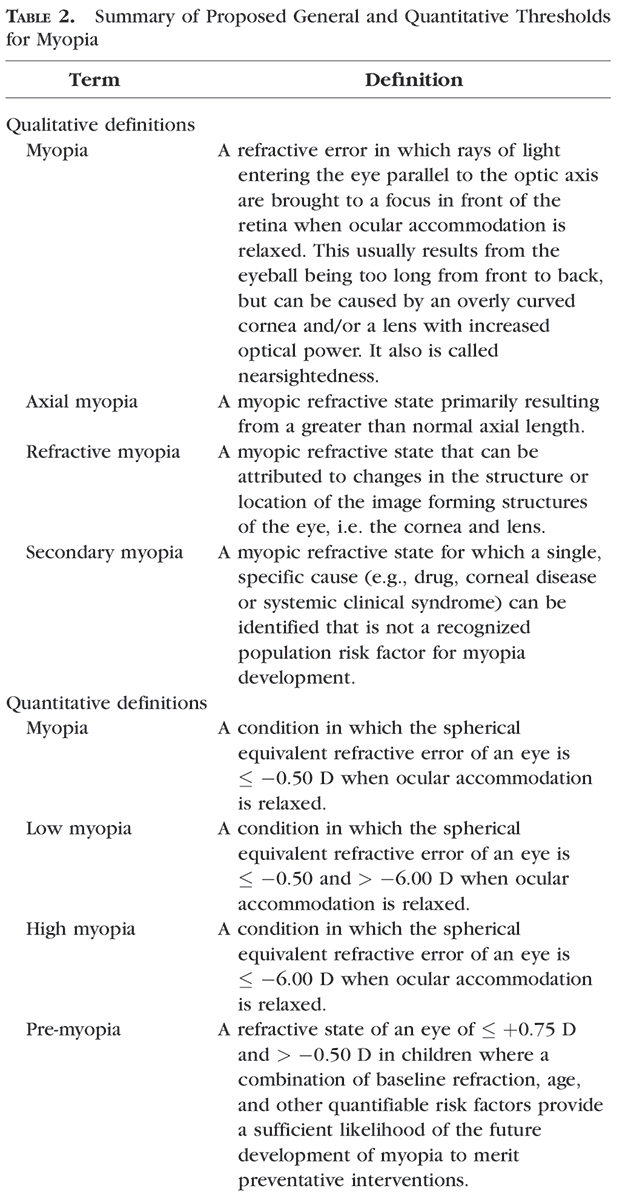
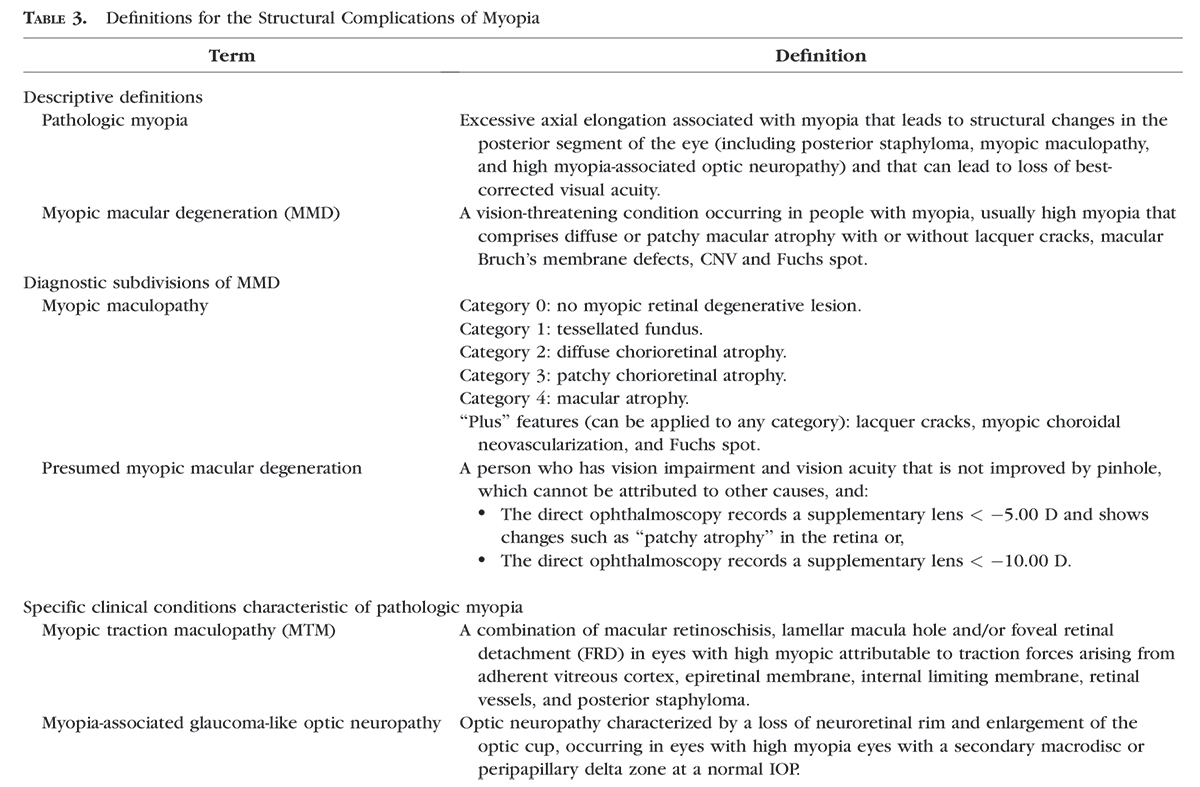
Currently, the extensive literature surrounding myopia has numerous, and often conflicting, definitions and an abundance of terms. Classifying myopia using inconsistent concepts and categories makes comparing research on the subject difficult. After extensive research and consideration, the International Myopia Institute (IMI) has released its proposal for a standardized set of terminology, definitions and thresholds of myopia and its main ocular complications. Two tables from the original paper summarizing its suggested nomenclature are included here. The institute believes that evidence-based, statistically sound and clinically relevant definitions will better serve future research in studying and managing the condition.
 |
| Courtesy of the Brien Holden Vision Institute. Originally published in Invest Ophthalmol Vis Sci. 2019;60:M20–M30. Click to enlarge. |
To develop the definitions and standards, the IMI included input from an international committee of researchers from the fields of pediatric ophthalmology, epidemiology, public health, optometry, clinical myopia research and medical retina. The committee wanted to ensure that homogenous groups of myopes could be easily selected for trials or genetic studies. Therefore, they differentiated myopia attributed to axial elongation from refractive myopia, where the changes are localized to the image forming structures of the eye, such as the cornea and/or lens.
The IMI recommend that the four descriptive categories of the condition are: myopia, secondary myopia, axial myopia and refractive myopia. They also differentiate myopia quantitatively into myopia, low myopia and high myopia. The institute states the current consensus threshold value for myopia is a spherical equivalent refractive error ≤-0.50 diopters (D) and the current consensus threshold value for high myopia is a spherical equivalent refractive error ≤-6.00D. ‘‘Pathologic myopia’’ is proposed as the categorical term for the adverse, structural complications of myopia, and “pre-myopia” is defined as “a refractive state of an eye of ≤ 0.75 D and > 0.50D in children where a combination of quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit preventative interventions.”
To establish a division into primary and secondary etiologies, the committee defined secondary myopia as “a myopic refractive state for which a single, specific cause (e.g., drug, corneal disease, or systemic clinical syndrome) can be identified that is not a recognized population risk factor for myopia development.”
The study also clarified that myopia must always be treated as a negative value and mathematical comparison symbols (e.g., <, >, ≤ and ≥) should only be used in their strict mathematical sense. This could help clarify ambiguities when comparing degrees of myopia.
High and Low
The IMI proposed that three quantitative categories, at a minimum, are required to describe the degree of myopia: myopia, low myopia and high myopia. Because high myopia is known to be associated with increased risks of visual loss, the committee believed that the threshold for it should also reflect this risk. Their definitions also avoid the requirement for objective refraction so as to be independent of technique; however by making reference to relaxation of accommodation, they are compatible with cycloplegic and standard clinical subjective techniques.
Myopia is defined as a condition in which the spherical equivalent refractive error of an eye is ≤-0.5 D when ocular accommodation is relaxed. When the spherical equivalent refractive error is ≤-0.5 and > -6.00D, it is considered low myopia. High myopia is defined as when the spherical equivalent refractive error is ≤6.00D.
 |
| Courtesy of the Brien Holden Vision Institute. Originally published in Invest Ophthalmol Vis Sci. 2019;60:M20–M30. Click to enlarge. |
Pathologic Myopia
The IMI decided that the more recognized “pathologic myopia” instead of the term in the World Health Organization’s International Classification of Diseases, “degenerative myopia” should describe excessive axial elongation that leads to structural changes in the posterior segment of the eye and also lead to best-corrected visual acuity loss. The committee also wanted to ensure that pathologic myopia could not be equated with high myopia. Myopic macular degeneration (MMD) is then proposed as the preferred categorical term for macular
The IMI conclude their study with their proposed criteria for adopting a clinical definition—relevance to nature of the research question, relevance to the underlying biology of myopia, acceptability to researchers in the field and use for developing public policy. The committee recognizes that some investigators may not adopt their definitions and categories, but they strongly urge that those nonstandard qualifying terms be clearly defined against the proposed terms and thresholds. Also, the results of those studies should involve both the chosen and standard thresholds whenever possible to make it easier to compare with other studies.
| Flitcroft DI, He M, Jonas JB, et al. IMI–Defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci. 2019;60:M20-30. |


