A
weekly e-journal by Art Epstein, OD, FAAO
Off the Cuff: Misery and Medicamentosa
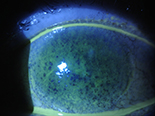
A delightful and intelligent 87-year-old woman was referred to me with a lengthy history of severe dry eye. This nice lady had traveled more than two hours each way to get to our office and as you can see below, after years of poor management, her eyes had been devastated. She shared that she often had agonizing pain, and I couldn’t help but think that after a long and productive life she didn’t deserve this. Then again, who does? I’ve found that sometimes the obvious remains obscure up until it hits you like a smack in the face. At her first visit I was perplexed by the four different glaucoma medications she was on, but at that moment my focus was on her ocular surface. I explained that I was concerned about the number of drops she was using, but that we would address her glaucoma management later, after we stabilized her dry eye. I prescribed an aggressive treatment regimen and saw her again several weeks later.
There are moments when you sit across from a patient and are moved by their suffering. You look into their eyes realizing you've tried nearly everything, but nothing seems to be working. Panic sets in. What do I do now? In that instant you realize you are it, and you have no choice but to do something. And you look again, and you think. Then, I suddenly recognized what I was really seeing. Beyond her dry eye, the combination of preserved drops she was taking multiple times a day was too much for her fragile cornea, and it was driving her severe surface disease. We modified her treatment using non-preserved medications and expect significant improvement.
|
||||||
 |
||
| Refractive Changes Induced By Strabismus Corrective Surgery in Adults | ||||
A retrospective chart review was conducted of adult patients who had horizontal recti muscle surgery with preoperative and postoperative cycloplegic refraction measurements to investigate refractive changes after strabismus correction procedures among adults. The preoperative refraction was mathematically subtracted from the postoperative refraction, and the induced refractive changes were statistically analyzed. Vector analysis was used to examine the magnitude of the toric change. The proportion of clinically significant refractive change was evaluated as well.
Thirty-one eyes from 22 subjects met the criteria and were included in the final analysis. A significant postoperative refractive change of the spherical equivalent towards myopia, and a change of the astigmatism in the with-the-rule direction, were observed. In a subset of nine cases, a third cycloplegic refraction measurement demonstrated stable refraction compared to the one-month postoperative measurement. In 10 cases of single eye surgery, significant refractive changes were observed only in the operated side when compared to the sound eye. The induced surgical refractive change was of clinical significance (≥0.5 D) in 11 eyes of nine patients (40.9% of patients). Researchers concluded that refractive changes were a significant side effect of horizontal strabismus corrective surgery among adults. Therefore, they advised that patients should be informed about these potential side effects prior to surgery and should be rerefracted in the postoperative period. |
||||
SOURCE: Mezad-Koursh D, Leshno A, Ziv-Baran T, et al. Refractive changes induced by strabismus corrective surgery in adults. J Ophthalmol. 2017;2017:2680204. 2017; Jan 16. [Epub ahead of print]. |
||||
 |
||
| Results of CNV Secondary to Pathological Myopia Treated with Ranibizumab | ||||
The current standard treatment of choroidal neovascularization (CNV) secondary to pathological myopia (PM) is intravitreal injection of VEGF antagonists, investigators wrote. They presented six-year results after treating patients with CNV secondary to PM with ranibizumab. Investigators retrospectively analyzed 15 treatment-naive eyes of 13 patients (10 women, 3 men; mean age: 59.2; standard deviation (SD): 11.1; range 41 years to 78 years) with visual impairment related to CNV secondary to PM, treated with at least one injection of ranibizumab. Follow-up treatments were indicated according to a pro re nata (PRN) regimen. Re-treatment criteria were: reduction in visual acuity and/or activity in OCT or fluorescence angiography. Patients received a mean of 3.5 ranibizumab injections (SD: 3.4; range 1 to 12) during a mean follow-up of 85 months (SD: 6.6; range 76 months to 102 months). Initial spherical equivalent was 12.4D ± 4.0D (range: 7.5D to 20.5D). Baseline visual acuity was (logMAR) 0.65 ± 0.28. After one month, visual acuity improved to 0.43 ± 0.23, after three months to 0.38±0.22, after six months to 0.34 ± 0.22 and after nine months to 0.35 ± 0.23. After one year, visual acuity was 0.35 ± 0.24, after two years 0.35 ± 0.23, after three years 0.35 ± 0.23, after four years 0.37 ± 0.23, after five years 0.38 ± 0.23 and after six years 0.39 ± 0.26. After considerable initial improvement in visual acuity, the initial gain was maintained by a strict PRN regimen for patients with neovascular membranes secondary to pathological myopia. The number of injections needed to achieve stable visual acuity was lower than with other diseases that respond to anti-VEGF, according to investigators. |
||||
SOURCE: Hefner L, Gerding H. Six-Year Results of CNV secondary to pathological myopia treated with ranibizumab. Klin Monbl Augenheilkd. 2017; Feb 13. [Epub ahead of print]. |
||||
|
||
| Clinical Features and Outcome of Pediatric Retinal Detachment | ||||
The aim of this study was to assess the clinical features and outcome of pediatric retinal detachment (RD). Ninety-five eyes of 87 children under 18 years of age with RD were assessed. The risk factors, morphology of RD, therapeutic approach and functional results were evaluated. Sixty-seven boys and 20 girls with a mean age of 10.4 years (standard deviation: 5.5) presented with RD. The following risk factors were identified: myopia (23%), congenital or developmental ocular abnormalities (37%), history of ocular trauma (40%) and previous ocular surgery (27%). Seventy-seven (81%) eyes underwent surgery. The primary reattachment rate was 44%. In 18%, reattachment was achieved after several surgeries. The overall recurrence rate after surgical reattachment was 39%. Researchers wrote that pediatric RD is a sight-threatening condition and that aggravating factors, such as delayed diagnosis, hereditary ocular abnormalities or strong vitreous adherence, are often present. They added that modern surgical techniques may contribute to a better outcome of RD in the future. |
||||
SOURCE: Barth T, Zeman F, Helbig H, et al. clinical features and outcome of paediatric retinal detachment. Ophthalmologica. 2017; Feb 11. [Epub ahead of print]. |
||||
 |
||
 |
||
| News & Notes | |||||||||
| Visiometrics Unveils New Website Visiometrics’ newly designed website improves the customer experience and makes it easier for providers and patients to find general product and technical information for the company’s HD Analyzer. Product information is supplemented with academic articles and video interviews featuring providers who use the system. An interactive quiz helps providers assess if they are good candidates for adding HD Analyzers to their practices. Finally, a dedicated patient page provides education materials to help providers explain the value of an HD Analyzer exam. Read more. |
|||||||||
| Growth Factor Shown to Protect Retina in Early Diabetes
Researchers from the Schepens Eye Research Institute of Massachusetts Eye and Ear have shown that a slight increase in transforming growth factor beta (TGF-β), present in preclinical animal models with diabetic eye disease, protects retinal blood vessels from diabetic retinopathy. Their findings, published online in the American Journal of Pathology, may lead to targeted therapeutics that delay or prevent the development of the disease. In light of these findings, the study authors recommend caution in the use of TGF-β blocking as a therapy for diabetes. Read more. | |||||||||
|
Optometric Physician™ (OP) newsletter is owned and published by Dr. Arthur Epstein. It is distributed by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073. HOW TO ADVERTISE |