A
weekly e-journal by Art Epstein, OD, FAAO
Off the Cuff: The High Cost of Better—An Eye Whitening Nightmare
The enemy of best is better, as my old friend and mentor Hank Perry would often say. Hank’s acquaintance with best and better came from years of experience as a meticulous corneal surgeon. In the decades since I first heard him say that, I’ve learned that this dictum was sagely advice. We all see patients complaining of chronic red, tired eyes. Often the cause is underlying meibomian gland dysfunction and dry eye disease. For some, the problem can be sufficiently disturbing to upturn a normal life. Many get addicted to Visine, while others seek more permanent solutions. For patients where better is not good enough, excessive trust and the promise of a quick fix can lead to catastrophe.
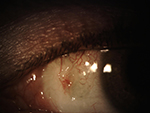
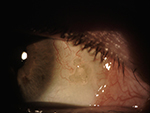
Over the past few years I’ve managed several patients who have undergone surgical eye whitening procedures. Perhaps it’s because I tend to see challenging patients, the ones I see have not had good outcomes. One otherwise beautiful young woman has gray uvea visible from beneath thinned patches of sclera. The other, a fastidious gentlemen with never a hair out of place, would give almost anything to get his old red eyes back. A quick look at the photos I captured today tell his story better than I can.
The surgery is similar to a procedure banned by the Korean Ministry of Health and Welfare in 2011 due to serious complications and multiple lawsuits. A large, retrospective study of the procedure published in the 2013 AJO reported a complication rate of 83%, with 56% considered serious. In March 2014, ASCRS issued a clinical alert because of the likelihood of serious complications, and reports of serious complications continue to be published in the US.
|
|||||||
 |
||
| Association Between Migraine and Dry Eye Disease | ||||
Despite the possible association between migraine and dry eye disease (DED), only a few studies investigate this link in a relatively limited number of patients. Therefore, researchers analyzed the relationship between migraine and DED in the Korean population. This population-based, cross-sectional study included 14,329 adults participating in the fifth annual Korea National Health and Nutrition Examination Survey from 2010 to 2012. Migraine, DED diagnosis and DED symptoms were assessed using questionnaires and surveys. Data were analyzed using logistic regression to determine the association of migraine with DED, while controlling for demographic, lifestyle and medical factors.
Individuals with migraine were more likely to report a DED diagnosis (14.4% vs. 8.2%) and DED symptoms (22.0% vs. 15.1%). In a multivariate analysis, the association between migraine and DED diagnosis was significant after adjustments. The association between migraine and DED symptoms showed a similar pattern. Although a causal relationship was not revealed, researchers found that patients who had a lifetime history of migraine were more likely to suffer from DED than individuals who did not present with headaches. However, they suggested that large, prospective, cohort studies would be needed to confirm the association between migraine and DED, as well as the influence of DED treatment on the frequency and severity of migraine attacks. |
||||
SOURCE: Yang S, Kim W, Kim HS, et al. Epidemiologic Survey Committee of the Korean Ophthalmologic Society. Association between migraine and dry eye disease. Curr Eye Res. 2017; Jan 27:1-5. [Epub ahead of print]. |
||||
 |
||
| Dry Eye Symptoms, Patient-Reported Visual Functioning and Health Anxiety Influencing Patient Satisfaction After Cataract Surgery | ||||
This study evaluated how patient satisfaction after cataract surgery is associated with postoperative visual acuity, visual functioning, dry eye signs and symptoms, health anxiety and depressive symptoms. Fifty-four patients (mean age: 68.02 years) were assessed two months after uneventful phacoemulsification; 27 were unsatisfied with their postoperative results and 27 were satisfied. They completed the following questionnaires: Visual Function Index-14 (VF-14), Ocular Surface Disease Index (OSDI), Shortened Health Anxiety Inventory (SHAI) and Shortened Beck Depression Inventory. Testing included logarithm of the Minimum Angle of Resolution (logMAR) uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA), dry eye tests (tear meniscus height and depth measured by spectral optical coherence tomography, tear film break-up time [TBUT], ocular surface staining, Schirmer 1 test and meibomian gland dysfunction grading). Postoperative UCVA, BCVA and the dry eye parameters, except TBUT, showed no statistically significant difference between the two groups. However, VF-14 scores, OSDI scores and SHAI scores were significantly worse in the unsatisfied patient group. No significant correlations were found between visual acuity measures and visual functioning. However, VF-14 scores correlated with OSDI scores, and OSDI scores correlated with SHAI scores. Multiple logistic regression revealed an adjusted association between patient satisfaction, and dry eye symptoms and visual functioning. The results suggested that patient-reported visual functioning, dry eye symptoms and health anxiety were more closely associated with patients' postoperative satisfaction than with the objective clinical measures of visual acuity or signs of dry eye. |
||||
SOURCE: Szakáts I, Sebestyén M, Tóth É, et al. Dry eye symptoms, patient-reported visual functioning, and health anxiety influencing patient satisfaction after cataract surgery. Curr Eye Res. 2017; Jan 27:1-5. [Epub ahead of print]. |
||||

|
||
| Effects of Latisse on the Ocular Surface | ||||
Latisse is marketed for the treatment of hypotrichosis (loss of eyelashes), using a prostamide analogue and preserved with benzalkonium chloride; however, it has also been reported to cause irritation to the ocular surface. Latisse is applied to the lid margin, but with the blink, some solution may fall onto the ocular surface. The objective of this study was to assess the effects of Latisse on the ocular surface over two months. Non-dry eye participants interested in eyelash lengthening were invited to a prospective, uncontrolled, open-label, clinical study using Latisse for two months. Eyelash length, subjective symptoms, tear film stability, osmolarity, ocular redness and intraocular pressure were evaluated at baseline (T0), and at one (T1) and two months (T2). Twenty-eight women (ages 18 to 29) entered the study. Fifteen completed the study, five discontinued it due to burning upon instillation and eight were lost to follow-up. Average eyelash length increased at each time. Dryness, burning and grittiness remained low (less than 25/100) throughout the trial with dryness showing a significant change between T0 and T1, but not between T1 and T2. No difference was noted for the noninvasive break-up time, photochromametry or tear osmolarity. Intraocular pressure showed a decrease with time but translated to only a 1mm Hg to 2mm Hg change, which was not clinically relevant. Investigators concluded that Latisse increased eyelash length within a short time (less than two months) and advised that patients seeking eyelash enhancement options should be educated as to appropriate use of the topical solution, precautions and any secondary effects, including the potential for discomfort upon instillation. |
||||
SOURCE: Bitton E, Courey C, Giancola P, et al. Effects of LATISSE (bimatoprost 0.03 per cent topical solution) on the ocular surface. Clin Exp Optom. 2017; Jan 25. [Epub ahead of print]. |
||||
 |
||
 |
||
| News & Notes | |||||||||
| Bausch + Lomb Partners with Popular TV Show for AMD Awareness Month Bausch + Lomb and Prevent Blindness are collaborating for the second year in a row during National Age-related Macular Degeneration Awareness Month in February to urge patients to spread the word about eye health and AMD through the #WhyEyeFight campaign. In an effort to reach patients in new and engaging ways, Bausch + Lomb has partnered with popular TV quiz show Jeopardy, which will kick off the month’s events with a special eye health category, set to air Feb. 7. (Check local listings to tune in.) This year’s campaign also includes a consumer-focused social media campaign so consumers can raise awareness and show support for the AMD community throughout the month of February. For every “share” or “like” of a Bausch + Lomb Facebook post promoting AMD Awareness Month, Bausch + Lomb will donate $1 to Prevent Blindness, up to $25,000. Consumers can also raise awareness by adding the #WhyEyeFight picture frame to their Facebook profile picture or share. Read more. |
|||||||||
| Alcon Releases Trifocal Toric Intraocular Lens
Alcon’s new AcrySof IQ PanOptix Toric presbyopia- and astigmatism-correcting intraocular lens for patients with pre-existing corneal astigmatism undergoing cataract surgery offers another option for astigmatic patients who want to address their near, intermediate and distance vision needs with a single lens. This IOL, which extends the PanOptix trifocal platform launched in September 2015, is intended for primary implantation in the capsular bag of the posterior chamber of the human eye for the visual correction of aphakia and pre-existing corneal astigmatism secondary to removal of a cataractous lens or clear lens. It is indicated for adult patients with and without presbyopia undergoing cataract surgery who desire near, intermediate and distance vision with increased spectacle independence. The IOL utilizes the same trifocal optic as the AcrySof IQ PanOptix IOL on the front surface of the lens and combines it with the astigmatic correction features of a toric IOL on the back surface. Read more. | |||||||||
|
Optometric Physician™ (OP) newsletter is owned and published by Dr. Arthur Epstein. It is distributed by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073. HOW TO ADVERTISE |