A
weekly e-journal by Art Epstein, OD, FAAO
Off the Cuff: Technology Matters
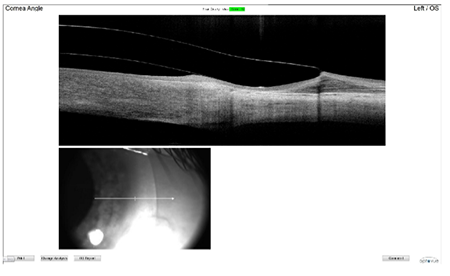
A few months ago, I wrote about the need for optometry to embrace technology before it steamrolled the profession into oblivion. Some elements of technology are self-evident. No one in their right mind would advocate managing a glaucoma patient using a tangent screen. Time tends to make things obsolete, and while tangent screens were state of the art in the 1970s, I suspect some of you may actually have to look up what a tangent screen is. Talking about glaucoma management, I could argue that OCT should be a standard of care. While that statement may make some uncomfortable, and yes, you can manage glaucoma patients without OCT, if you or your family member had glaucoma, how would you want to be managed? I can’t imagine having a successful dry eye specialty practice without meibography. I can’t imagine diagnosing or even fitting a keratoconus patient without using a topographer. Yet some still do it. Let me share a concrete example of why old school approaches are rapidly becoming obsolete. This patient was fitted four months ago elsewhere and, with 20/50 BCVA, was told that that was the best that could be done. The patient complained that the lens was achy and painful. For those not familiar with scleral lenses, most patients find them to be as, if not more, comfortable than soft lenses. The first (Optovue iVue) OCT image, immediately below, is of the scleral lens the patient was wearing when they arrived. Even if you’re unaccustomed to viewing OCTs of scleral lens fits, it’s easy to see why the patient was miserable. The picture says it best, but the fit was atrocious. The lens was fitted using fluorescein.
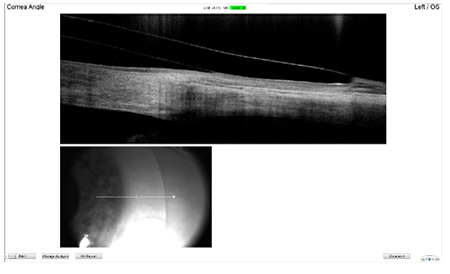
The second image below was of the Zen trial lens that Shannon fit. BCVA with the trial lens was 20/20. Again, the picture tells the story best, but it can’t capture the relief and how much more comfortable the patient was.
There was a time about 30 years ago, when working with world-class cornea specialists and mentors Hank Perry and Eric Donnenfeld that they replaced their old Corneascope with a brand new Tomey TMS-1 topographer. My initial reaction was, who needs that? I can get a just fine idea of corneal shape with a large GP and fluorescein. Boy was I wrong. Nothing against fluorescein. I use it all the time, but if I was being fitted with a scleral lens or being managed for glaucoma, I would prefer my doctor used modern technology. Hindsight may be 20/20, but foresight is even better.
|
|||||||
 |
||
| Ocular Surface Changes in Hashimoto's Thyroiditis Without Thyroid Ophthalmopathy | ||||
Researchers sought to evaluate ocular surface changes in patients with Hashimoto's thyroiditis without thyroid ophthalmopathy to elucidate the relationship between dry eye syndrome and meibomian gland dysfunction (MGD) in cases of Hashimoto's thyroiditis. This prospective study included 105 patients with Hashimoto's thyroiditis and 105 age- and sex-matched controls. The 12-item Ocular Surface Disease Index (OSDI) questionnaire was administered to all patients. Both eyes affected by Hashimoto's thyroiditis and normal eyes were evaluated and compared with regard to the following parameters: Hertel exophthalmometry, palpebral fissure height, tear-film breakup time (TBUT), Schirmer 1 test, area and density scores for corneal fluorescein staining, eyelid abnormality, meibomian gland expression, meibography scores and areas of meibomian gland loss. The eyes affected by Hashimoto's thyroiditis demonstrated significantly lower TBUTs, Schirmer 1 test scores and meibomian gland expression, and significantly higher OSDI scores, corneal fluorescein staining results, eyelid abnormality scores, meibography scores and areas of meibomian gland loss. Ocular Surface Disease Index scores were significantly positively correlated with eyelid abnormality scores, meibography scores and areas of meibomian gland loss, and negatively correlated with meibomian gland expression. The duration of Hashimoto's thyroiditis was significantly positively correlated with MGD. Researchers wrote that dry eye syndrome and ocular discomfort symptoms were significantly more common among patients with Hashimoto's thyroiditis, even in the absence of thyroid ophthalmopathy. They added that dry eye syndrome in patients with Hashimoto's thyroiditis is believed to result from MGD and is correlated with the duration of the thyroid disease.
|
||||
SOURCE: Altin Ekin M, Karadeniz Ugurlu S, Egrilmez ED, et al. Ocular surface changes in Hashimoto's thyroiditis without thyroid ophthalmopathy. Eye Contact Lens. 2020; Feb 24. [Epub ahead of print]. |
||||
 |
||
| The ABCs of Ocular Trauma: Adapting a Familiar Mnemonic for Rapid Eye Exam in the Pre-ophthalmic Zone of Care | ||||
Evaluation and management of eye trauma is daunting to many practitioners. For general medical emergencies, the familiar ABCs mnemonic serves to both recompose the provider as well as provide a logical order for evaluation and action. We recently adapted an ABCs mnemonic to provide non-ophthalmologists with a familiar method for systematically evaluating and managing eye trauma. A=ACUITY. Visual acuity is the most important piece of information in eye trauma. B=BEST exam of BOTH eyes. Starting with acuity, examination proceeds from the front to the rear of the eye. Examine the uninjured eye first. C=CONTIGUOUS STRUCTURES and CONTACT LENSES. Examine structures contiguous to the apparent injury. Inspect for contact lens wear. D=DRUGS, DIAGNOSTIC IMAGING and the DON'TS. Start antibiotics, antiemetics and analgesics. Administer tetanus. Obtain computerized tomography if available. Do not attempt ocular ultrasound or magnetic resonance imaging. Do not apply pressure to the eye. Do not patch the eye or apply any medication. E=EYE SHIELD and EVACUATE. Shield and ship to ophthalmology. The mnemonic was adapted to reflect current Joint Trauma Services and Tactical Combat Casualty Care practice guidelines. The authors believe this familiar mnemonic can serve as a useful tool in enabling non-ophthalmologists to comfortably and safely evaluate an eye for trauma. |
||||
SOURCE: Kroesen CF, Snider M, Bailey J, et al. The ABCs of ocular trauma: adapting a familiar mnemonic for rapid eye exam in the pre-ophthalmic zone of care. Mil Med. 2020;185(Supplement_1):448-53. |
||||
 |
||
| Ganglion Cell Complex Analysis in Glaucoma Patients: What Can it Tell Us? | ||||
Glaucoma is a group of optic neuropathies characterized by a progressive degeneration of retinal ganglion cells (RGCs) and their axons that precedes functional changes detected on the visual field. The macular ganglion cell complex (GCC), available in commercial Fourier-domain optical coherence tomography, allows the quantification of the innermost retinal layers that are potentially involved in the glaucomatous damage, including the retinal nerve fiber (RNFL), ganglion cell and inner plexiform layers. The researchers wrote that the average GCC thickness and its related parameters represent a reliable biomarker in detecting preperimetric glaucomatous damage. Further, they added, the most accurate GCC parameters are represented by average and inferior GCC thicknesses, and they can be associated with progressive visual field loss. Although, they noted, that the diagnostic accuracy increases with more severe glaucomatous damage and higher signal strength values, it is not affected by increasing axial length, resulting in a more accurate discrimination of glaucomatous damage in myopic eyes with respect to the traditional RNFL thickness. The researchers reported that the analysis of the structure-function relationship reveals a good agreement between the loss in retinal sensitivity and GCC thickness. They noted that the use of a 10-2 degree visual field grid, adjusted for the anatomical RGCs displacement, describes more accurately the relationship between RGC thickness and visual field sensitivity loss. |
||||
SOURCE: Scuderi G, Fragiotta S, Scuderi L, Iodice CM, et al. Ganglion cell complex analysis in glaucoma patients: what can it tell us? Eye Brain. 2020;12:33-44. |
||||
 |
||
| News & Notes | ||||||||
| Alcon to Launch Pataday Following FDA Approval of OTC Switch Alcon announced the FDA approved Pataday Once Daily Relief (olopatadine hydrochloride ophthalmic solution 0.2%) and Pataday Twice Daily Relief (olopatadine hydrochloride ophthalmic solution 0.1%) for over-the-counter sale in the US. The Pataday brand features the first once-daily allergy itch relief drop to be available without a prescription. The rights to the Rx-to-OTC switch were secured by Alcon as part of its separation from Novartis in April 2019. Read more.
|
||||||||
| J&J Vision Issues Worldwide Call to Prioritize Your Eyes in 2020 Johnson & Johnson Vision announced the launch of Prioritize Your Eyes, a worldwide effort to raise awareness about the connection of eye health to overall health. Prioritize Your Eyes encourages everyone to take the most important step to protect their eyes—getting an eye exam—and is part of the company’s ongoing commitment and collaboration with various partners and professional organizations to elevate eye health and make 2020 the year of greater eye health awareness. Read more. |
||||||||
| Eyevance Appoints Speed as Chief Commercial Officer Eyevance Pharmaceuticals announced the appointment of Julie Speed as chief commercial officer. Speed will be responsible for developing the commercial strategy and overseeing growth of Eyevance’s product portfolio Speed previously worked at Johnson & Johnson Vision, TearLab and Alcon. Read more. |
||||||||
| RightEye Reveals 2020 Impact Award Finalists RightEye revealed the six finalists of its 2020 RightEye Impact Awards. The grand prize winner will be honored at a March 13 ceremony in the winner’s hometown. 1. Dr. Sally Fryer Dietz, Integrative Concussion & Pediatric Therapy, Dallas, TX 2. Debra Holtzhauer, Listowel Vision Care, Listowel, Ontario, Canada 3. Jeremiah Jorgensen, Fyzical Therapy and Balance Centers, Lincoln, NE 4. Dr. Amanda Nanasy, Florida Institute of Sports Vision at The Eye Center, Pembroke Pines, FL 5. Dr. Neil Renaud, EagleEye Performance Vision, Holland, MI 6. Dr. Gregory Schultz, Eye Center of Virginia, Williamsburg, VA Read more. |
||||||||
|
||||||||
|
Optometric Physician™ (OP) newsletter is owned and published by Dr. Arthur Epstein. It is distributed by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073. HOW TO ADVERTISE |