A
weekly e-journal by Art Epstein, OD, FAAO
Off the Cuff: The Important Things
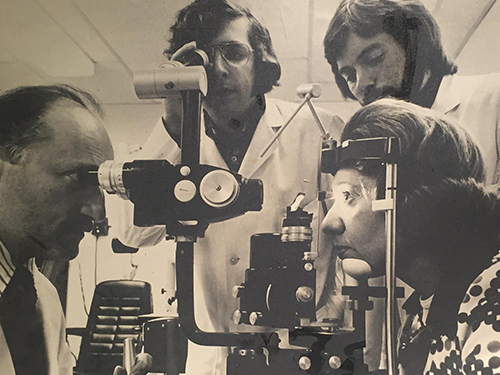
This was not a particularly good week for optometry. I had planned on sharing some of these pressing issues, but decided against it. I realized I had other things I wanted to say. I decided to write about some of the truly important things—the bonds of friendship, pride in others and how important we can be in other people’s lives.
One treat for me at these events is that I always connect with friends from around the country. Such was the case in Philly, but two things made this last B+Lieve event of the year truly special. First, my best friend from optometry school, Harold Schiff, was there. Incredibly, we didn’t skip a beat. After all of these years, we were still as strongly connected as we were when we rode the F train together into school each morning. We shared stories about our families and talked about old times. It was great!
|
||||||
|
||
| The Impact of Scleral Contact Lens Vault on Visual Acuity and Comfort | ||||
This study assessed how varying degrees of corneal clearance of scleral contact lenses (ScCL) impact visual acuity (VA) and comfort in patients with corneal ectasia. Three ScCL were fitted to 20 subjects with previous diagnosis of either keratoconus (n=18) or pellucid marginal degeneration (n=2). Fitting of ScCL was based on corneal sagittal height (CSH) measured with Visante OCT at a 15-mm chord on the horizontal meridian. To select the ScCL from the diagnostic lens set, values of 325μm, 375μm and 425μm were randomly added in sequence to CSH. Subjects wore ScCL for one hour. Central corneal clearance (CCC) and topographic corneal clearance (TCC) along the vertical meridian were assessed using an ultralong optical coherence tomographer. High-contrast VA (HCVA) and low-contrast VA (LCVA) were measured using a logarithm of the minimum angle of resolution VA chart, and comfort ratings were obtained with a standard comfort scale (zero to 100).
Mean CSH in the horizontal meridian was 3.78mm ± 0.53mm (range: 3.33 to 4.17) at a 15-mm chord. Mean CCC was 190μm ± 100μm (TCC: 160μm ± 94μm at +3mm; and 180μm ± 94μm at -3mm), 360μm ± 120μm (TCC: 260μm ± 100μm at +3mm; and 330μm ± 110μm at -3mm), and 450μm ± 170μm (TCC: 320μm ± 120μm at +3mm; and 400μm ±120μm at -3mm) for each lens. The mean HCVA for lenses one, two and three were 0.05 ± 0.12, 0.07 ± 0.11 and 0.11 ± 0.08 respectively, which were significantly different. Tukey post hoc analysis showed that this difference was only significant between lenses one and three. Similar findings were found for LCVA. Comfort ratings for lenses one, two and three were 74.9 ± 9.2, 79.7 ± 11.6 and 78.6 ± 10.8, respectively. Researchers concluded that using CSH measurements was an effective method for determining the appropriate lens/cornea relationship. Lens two (+375μm) gave the best combination of acuity and comfort ratings. Researchers added that evaluation of the fluorescein pattern must be balanced with VA and comfort ratings for successful fitting in a clinical setting. |
||||
SOURCE: Otchere H, Jones L, Sorbara L. The impact of scleral contact lens vault on visual acuity and comfort. eye contact lens. 2017; Sep 26. [Epub ahead of print]. |
||||
 |
||
| Assessment of Eye Drop Instillation Technique in Glaucoma Patients | ||||
In this cross-sectional study, 71 consecutive patients with glaucoma or ocular hypertension, self-administering topical anti-glaucoma medications for ≥6 months were evaluated to study the technique of eye drop instillation in glaucoma patients and identify independent factors that may influence performance. All patients instilled a tear substitute into the eye with the worst eyesight using the technique normally used at home. The following parameters were evaluated: age, number of years receiving treatment with ocular hypotensive eye drops, time spent to instill the first drop, number of drops instilled, correct location of the eye drops, contact of the bottle with the eye, closing of the eyelids or occlusion of the tear punctum, and asepsis of the hands.
The mean age of the patients was 66 ± 10.8 years, and patients were on ocular hypotensive drugs for 11.3 ± 7.3 (range, 2 to 35) years. Only 28% of patients were able to correctly instill the eye drops (squeeze out one drop and instill it into the conjunctival sac without bottle tip contact). Touching the tip of the bottle to the globe or periocular tissue occurred in 62% of patients. In 49% of patients, the eye drops fell onto the eyelids or cheek. Two or more drops were squeezed by 27% of patients. The majority of glaucoma patients were unable to correctly instill eye drops. Age was an independent factor associated with eye drop instillation performance. |
||||
SOURCE: Gomes BF, Paredes AF, Madeira N, et al. Assessment of eye drop instillation technique in glaucoma patients. Arq Bras Oftalmol. 2017;80(4):238-41. |
||||
|
|||
| Glaucoma, Depression and Quality of Life: Comorbidities and Assessments, and Multidisciplinary Plan Treatment | ||||
This review evaluated the assessment and comorbidity of glaucoma and depression with the possibility of treatment options. The web of science was searched for relevant articles using the search terms: "glaucoma," "depression," "glaucoma and depression" and "quality of life and glaucoma." Additional relevant papers were added from the bibliography of selected papers. All types of articles were included, and no time period was defined.
Authors reviewed 11 studies regarding the comorbidities of glaucoma and depression. The number of participants in all studies ranged from 86 to 6,760. The scale formats were self-reported in all but one study, which was clinician-rated. Two studies explored types of glaucoma. Three out of 11 revealed no significant evidence of elevated depressive symptoms associated with glaucoma. In six studies, the prevalence of depression was significant among glaucoma patients. One study provided suboptimal assessments of depression in glaucoma patients. Another showed the presence of glaucoma significantly associated with depression after adjustment for demographic factors. Most of the studies used one scale, while two used two scales. The reviewed studies did not analyze the therapy options of included patients. The results indicated that glaucoma was accompanied by depression in the majority of analyzed studies. Authors wrote that the comorbidity of glaucoma and depression should be the subject of further research involving self-reflecting and clinician-rated scales, taking into account the subjective experience of patients and physicians. They added that therapy options should be assessed in future research, including novel possibilities for treating both conditions respectively. |
||||
SOURCE: Pelčić G, Ljubičić R, Barać J, et al. Glaucoma, depression and quality of life: multiple comorbidities, multiple assessments and multidisciplinary plan treatment. Psychiatr Danub. 2017;29(3):351-9. |
||||
 |
||
| News & Notes | |||||||||
| NaturalVue Multifocal Lens Research: Myopia Reversal in Animal Model The NaturalVue Multifocal 1 Day Contact Lens design was recently shown to fully reverse previously induced myopia in an animal model (chickens), according to research published in the September edition of Ophthalmic and Physiological Optics. The study, supported in part by a grant from Visioneering Technologies, was a follow-up to milestone research published by lead author Elizabeth L. Irving, OD, PhD, professor, University Research Chair, University of Waterloo, that showed that the lens design was able to fully stop the development of up to 10D of myopia in the same animal model. Read more.
|
|||||||||
Pentacam AXL Integrates Barrett Formulas
|
|||||||||
| Aerie Announces FDA Advisory Committee Meeting for Rhopressa The U.S. Food and Drug Administration’s Dermatologic and Ophthalmic Drugs Advisory Committee was scheduled for Oct. 13, to review Aerie Pharmaceuticals’ New Drug Application for Rhopressa (netarsudil ophthalmic solution) 0.02% for the treatment of individuals with open-angle glaucoma or ocular hypertension. Aerie submitted the NDA in February 2017, after which the FDA set a Prescription Drug User Fee Act goal date of February 28, 2018, for completion of its NDA review. Read more. |
|||||||||
Eyevance Enters into Licensing Agreement for Zerviate in the United States
|
|||||||||
| Alfred A. Rosenbloom, Jr., Low Vision Residency Award Recipient Chosen Rachel Young, OD, a low vision, traumatic brain injury, and primary care resident at the VA Long Beach Medical Center, was chosen by a committee of members in the Low Vision Section of the American Academy of Optometry as this year’s recipient for the Alfred A. Rosenbloom, Jr., Low Vision Residency Award. Young will receive a $2,000 education award and a $750 travel fellowship to attend the Academy 2017 Chicago annual meeting in October. Read more.
|
|||||||||
AAOF Releases Johnson & Johnson Vision Residency Award Recipients
|
|||||||||
AAOF Selects Beta Sigma Kappa Research Fellowship Recipient
|
|||||||||
Fredric Rosemore Low Vision Grant Recipient Named
|
|||||||||
|
Optometric Physician™ (OP) newsletter is owned and published by Dr. Arthur Epstein. It is distributed by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073. HOW TO ADVERTISE |