
Dr. Mangan presented urgent cases from the strange to the scary in yesterday’s course on ocular emergencies. |
|
Emergency Protocols in Optometry
When patients stick their noses—or eyes—where they don’t belong, ODs must act fast.
Black humor enthusiasts are well aware of the Darwin Awards—an unofficial listing of the dumbest ways people have injured themselves each year. Rich Mangan, OD, kept the crowd of his pre-lunch presentation “Be Prepared! Handling Ocular Emergencies” engaged with reminders that people often make risky choices; photos of ladders propped up on wheeled garbage cans, motorcyclists treating their moving vehicle like a La-Z-Boy and even a video of a marksman checking the barrel of his firearm only to have it nearly blow his nose off.
Dr. Mangan, who writes Review of Optometry’s Urgent Care column, even offered a collection of cases he’s witnessed that may offer an optometric analog to the Darwins, such as patients who have stored soft contact lenses in pond water, shot themselves in the eye with paintball guns and even enucleated their own eyes. Call them the “Mangan Awards” perhaps, but the speaker also offered careful guidance on how attendees can treat these patients.
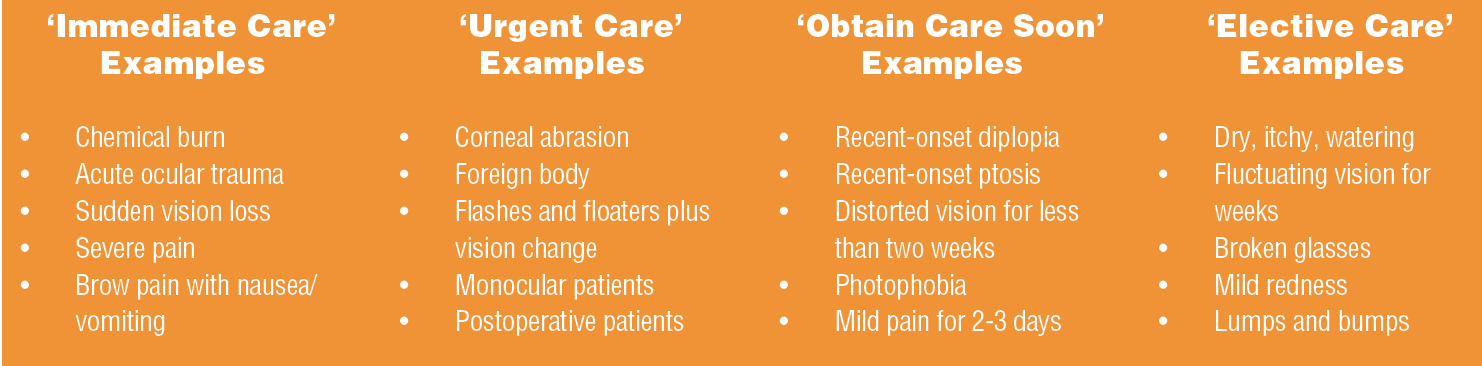
The first step, Dr. Mangan said, is identifying whether or not your patient has a true ocular emergency, and if it needs to be treated immediately (within a matter of hours), urgently (within a day), soon (within a week) or on an elective basis (within a month). Making that call begins with training staff to understand “the art of triage,” Dr. Mangan said. “It’s defined as sorting patients according to the urgency of their need for care.”
The presentation consisted of a number of case examples to demonstrate how ODs can manage ocular emergencies.
You’re So Vein
Patients with ocular trauma may not realize it, but some of their symptoms may indicate that they’re experiencing a central retinal artery occlusion. Fundus imaging, however, will reveal the damage to their vascular system. Be on the lookout for superficial opacification or whitening of the retina in the posterior pole with a cherry-red spot in the center of the macula, Dr. Mangan said, and if you suspect it, act immediately. “When you go outside a four-hour window, your prognosis is really, really poor,” he explained, but “it’s still recommended, even within a six- to eight-hour time frame, that you try to re-perfuse the eye.” Dr. Mangan said not to spend precious time taking a complete family history in these cases—treat first. That intervention can include anything from orbital massage to anterior paracentesis to a special Nd:YAG laser application. The goal here is to reduce the pressure on the eye.
Burn, Baby, Burn
“There are some chemicals that can eat through a cornea, or the eye, in only five minutes,” he warned. Alkali-based chemicals are more severe than acid-based ones, but Dr. Mangan said all contingencies, such as how much of the chemical got in the eye and how long ago it happened, play a role. Sixty percent of these types of burns occur at work, but plenty of household items contain dangerous chemicals, and children are especially prone to this type of injury. For these cases, management needs to begin over the phone because “you want to start irrigation right away,” he said. Instruct the patient to find a shower or even an outdoor hose. Don’t even try to take contact lenses out, he noted. Just keep irrigating. Also, don’t forget to ask patients to bring the container that held the chemical if they’re not sure what it was.
Once they arrive at the office, refer to the Roper-Hall classification of ocular surface burns to judge how to start treatment. “If it’s a basic substance or an alkali burn, you may want to avoid a topical glaucoma drop and use an oral instead,” Dr. Mangan said. And “if there’s any kind of limbal blanching, I think the patient will benefit from a Prokera amniotic membrane (Bio-Tissue). Sometimes I’ll wait until three to five days out from the burn and assess the healing. If the healing is a little slow, I’ll turn to the Prokera.”
Not-so-gentle Giant
In cases of giant cell arteritis, if they’re in your chair, chances are they’ve already lost vision in at least one eye. “Clearly, if they’ve already had vision loss in one eye, this is a true ocular emergency,” Dr. Mangan said. And if there’s any doubt, get a blood test. “It’s urgent we get these patients started on steroids right away,” he said. Other treatments include obtaining a biopsy, but even that’s not 100% reliable. The American College of Rheumatology offers a five-point scoring system. If your patient has any three of these, you’re justified in starting steroids:
Older than 50 years of age.
A Westergren ESR greater than 50.
Temporal artery tenderness or abnormality on exam.
New-onset headache.
Positive temporal artery biopsy.
Soft Cell
One patient presented to Dr. Mangan complaining of a “pulling” sensation in his left eye when looking superior temporal. The diagnosis turned out to be periorbital cellulitis, an infection usually caused by Staphylococcus or Streptococcus.
For patients with tenderness, proptosis and blurred vision, he said, ask if they’ve had any surgeries, such as lid and sinus surgeries (or a history of trauma), because patients who’ve undergone these can get infections even months to years later. Unlike with chemical burns, “you want to get as much of a history as you can” to uncover the cause of the infection.
Initial treatment will include antibiotics, but if the problem persists, patients may need to undergo a particularly gory procedure that requires a surgeon to “push out the pus.” A video of this elicited uncomfortable groans, even from this room full of doctors.