 |
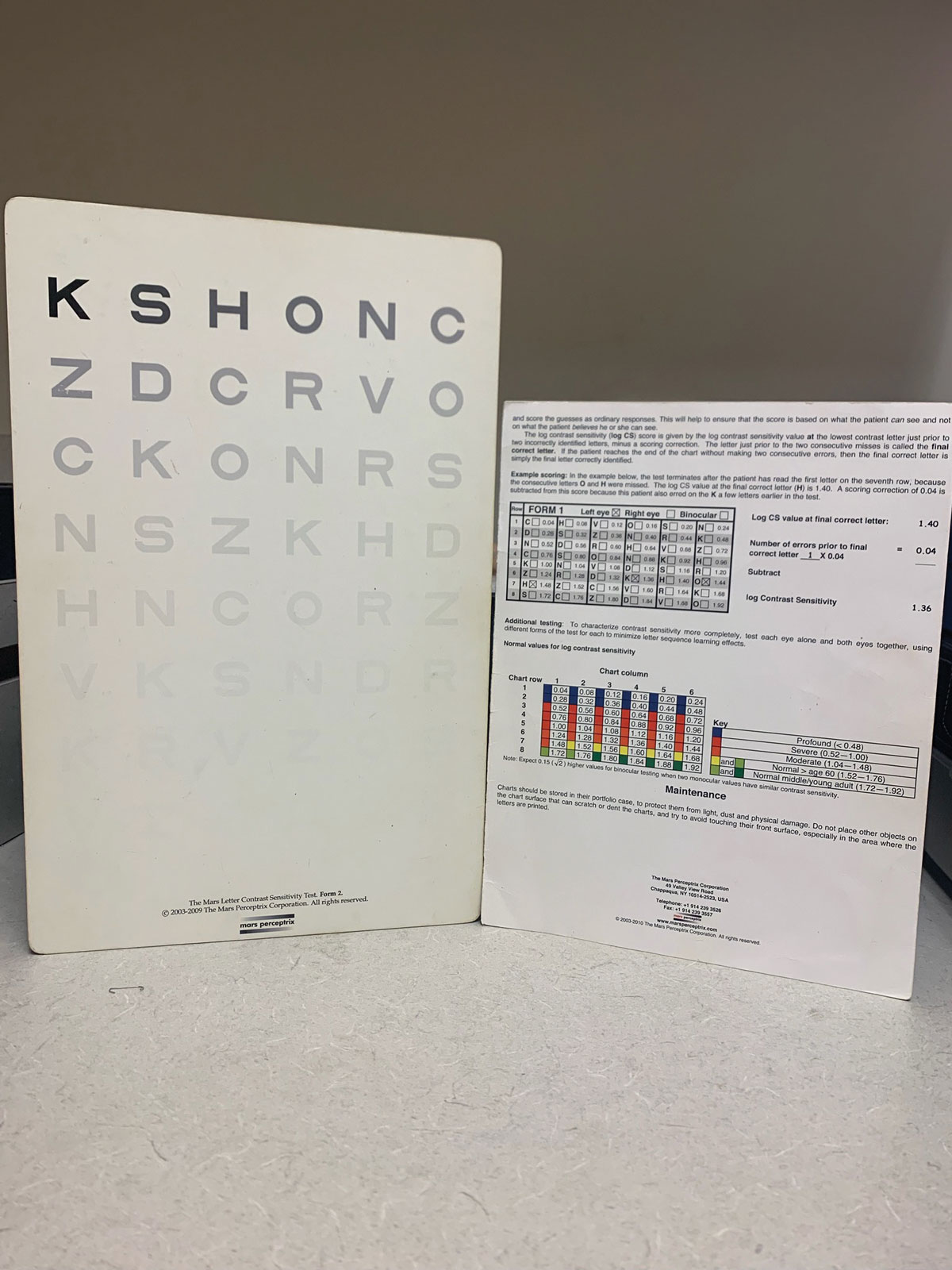
| While contrast sensitivity alone is not sufficient to identify people with eye disease, it is an important measure of visual function that can add value to comprehensive eye screenings. Photo: Bisant A. Labib, OD. Click image to enlarge. |
Some studies have speculated that contrast sensitivity (CS) may give clinicians an early indication of vision difficulties not yet detectable by visual acuity (VA) measurement alone. To explore that idea, University of Michigan researchers recently investigated the value of contrast sensitivity as a screening tool to detect eye diseases and gauge vision-related quality of life (VRQOL). It has some merit, they found, but can’t be relied upon to uncover disease.
A total of 1,159 participants received a vision exam reviewed via telemedicine, completed a demographic survey and the nine-item Visual Function Questionnaire (VFQ-9). The ability of contrast sensitivity to predict eye disease was explored and area under the curve was reported. Logistic and linear regression were used to investigate the probability of screening positive for eye disease and VFQ-9 score, respectively, adjusting for age and VA.
The relationship between VRQOL and contrast sensitivity in this study is similar to previous work showing its importance as it relates to VRQOL in diseases such as cataract, AMD, diabetic retinopathy and glaucoma. “In previous research among glaucoma patients, lower CS in the better eye was associated with worse VRQOL, but lower CS in the worse eye was not, meaning that if the better eye was more compromised in terms of CS, people felt more visually compromised,” the authors noted in their paper for American Journal of Ophthalmology.
Asymmetry plays a role in VRQOL, they found, as a larger difference in contrast sensitivity between eyes was significantly correlated with a decrease in visual function measured by the VFQ-9 composite score. Additionally, larger CS asymmetry was associated with worse VRQOL in five of the seven subscales of the VFQ-9: general vision, distance activities, mental health, driving and peripheral vision.
“The findings that a larger difference in contrast sensitivity between the better and worse eye is associated with decreased VRQOL suggests that contrast sensitivity is an important aspect of visual function that cannot necessarily be compensated for by the eye with a better contrast sensitivity,” the authors wrote. “In clinical practice, it is common to focus attention on the better-seeing eye if a patient has a large difference in VA between eyes. These results give pause to that approach and may help inform choices in low-vision rehabilitation in terms of focusing some efforts on rehabilitating the worse-seeing eye as well.”
The authors emphasized that it’s important to contextualize the magnitude of the relationship between contrast sensitivity and VRQOL. “For example, in patients with newly diagnosed open angle glaucoma, previous work has shown that the minimally important clinical difference in VA (a 10-letter difference on the Snellen chart) is associated with a 3.8 unit decrease in VFQ-9 score,” they explained. “In terms of our findings, a one-line decrease in better eye contrast sensitivity (0.3 log unit) was associated with a 5.9 unit decrease in the VFQ-9 composite score and a one-line decrease in worse eye contrast sensitivity was associated with a 3.9 unit decrease in the VFQ-9 composite score, after adjusting for age and VA. A one-line reduction in contrast sensitivity in the better seeing eye has more impact on VRQOL than a two-line decrease in VA, demonstrating the importance of contrast sensitivity in people’s visual function.”
In conclusion, contrast sensitivity gives insights into a patient's visual function and quality of life but lacks diagnostic specificity.
“While our study found that measuring contrast sensitivity using the Pelli-Robson chart was not sensitive or specific enough to be used in screening for eye disease, it was a valuable tool in assessing visual function,” the authors explained. “These findings highlight the potential utility in measuring contrast sensitivity in addition to VA in routine eye examinations or in times when visual complaints are not adequately captured by VA.”
Flaharty K, Niziol LM, Woodward MA, et al. Association of contrast sensitivity with eye disease and vision-related quality of life. Amer J Ophthalmol. January 19, 2024. [Epub ahead of print.] |


