 |
|
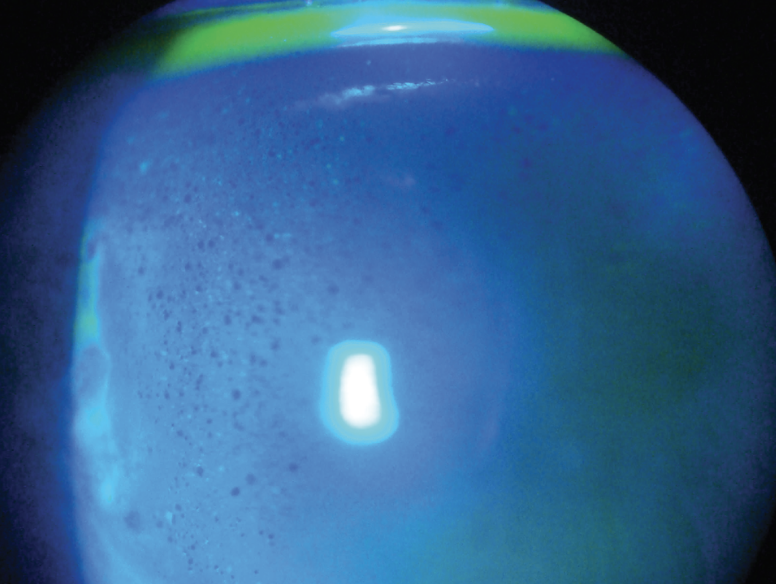
In diabetic patients, having macular edema increased the chances of corneal edema. However, the study noted that diabetic retinopathy severity, diabetic kidney disease and the presence of peripheral circulatory disease were not associated with increased odds of corneal edema. Photo: Michal Reygan Martin, OD. Click image to enlarge. |
While cataract and refractive surgical procedures have evolved tremendously in recent decades, postoperative corneal edema is still somewhat commonly present. Researchers at the Icahn School of Medicine at Mount Sinai in New York City studied which factors increase the risk of developing corneal swelling and which patients eventually required corneal transplantation after cataract surgery. Their study, whose findings were presented at ARVO in Seattle earlier this week, demonstrated that people with diabetes were more likely to have corneal edema after surgery. Older individuals also had a higher risk, and this risk increased with age. Notably, different racial and ethnic groups had a higher likelihood of developing corneal edema and needing a corneal transplant compared with Caucasian patients.
The researchers collected data from a nationwide sample of Medicare beneficiaries 65 years old and older who received cataract surgery. In 192,150 patients with at least one year of follow-up, age, gender, race/ethnicity, tobacco use and hypertension diagnosis were collected. Multivariable logistic regression models then assessed the relationship between demographic factors and diabetic sequelae on the development of corneal edema and the subsequent need for corneal transplantation.
|
For more on post-op edema, see this recent article. |
Patients with diabetes were more likely to develop corneal edema compared with non-diabetic patients after cataract surgery (odds ratio [OR]: 1.25). Compared with patients aged 65 to 74, patients aged 75 to 84 (OR: 1.38) and over 85 (OR: 2.40) were more likely to develop corneal edema. Compared with Caucasian patients, Black, Asian, Hispanic and North American Native patients were significantly more likely to develop both corneal edema (ORs: 1.75, 2.69, 2.80 and 3.32, respectively) and eventually require corneal transplantation (ORs: 1.99, 4.32, 4.81 and 6.35, respectively). Female patients had lower odds of requiring corneal transplantation postoperatively (OR: 0.53).
In these patients, the presence of macular edema was associated with increased odds of developing corneal edema (OR: 1.86). However, the researchers found that the severity of diabetic retinopathy, diabetic kidney disease and the presence of peripheral circulatory disease were not associated with increased odds of corneal edema.
The researchers concluded that more research is needed to understand why certain racial and ethnic groups in the US face a significantly increased risk of these complications.
Original abstract content @2024 Association for Research in Vision and Ophthalmology.
Li G, Sommi A, Klawe J, Ahmad S. Risk factors for corneal decompensation in diabetic and non-diabetic patients after cataract surgery. ARVO 2024 annual meeting. |


