 |
| Visual field progression is most likely to progress in patients with ocular hypertension in the nasal and paracentral regions of the optic disc, and treatment may slow the rate, according to a new study. Photo: Austin Lifferth, OD. Click image to enlarge. |
Ocular hypertension is one of the most significant risk factors for developing primary open-angle glaucoma (POAG). The landmark Ocular Hypertension Treatment Study demonstrated how this disease converts to POAG, and the extensive data collected presented other researchers with the chance to look for patterns of visual field (VF) loss.
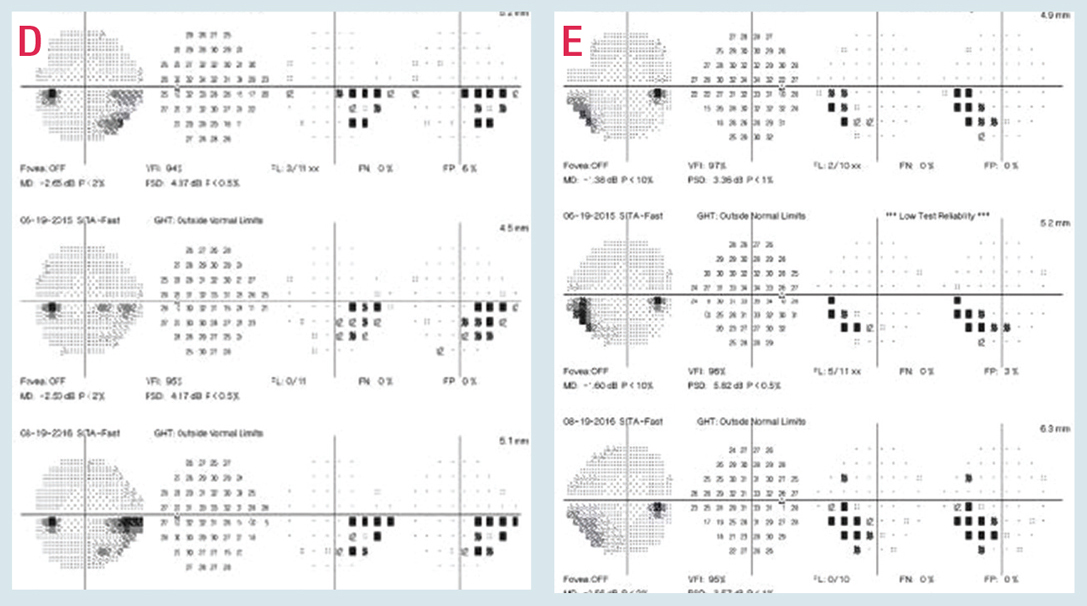
Armed with this information, the authors of a new study say they’ve identified the nasal and paracentral regions as being more prone to a reduction in sensitivity in patients with ocular hypertension (OHTN). These results included both event- and trend-based analyses, and was observed in both the early- and delayed-treatment groups.
Authors included over 2 million test points from 58,115 visual fields of 1,188 patients who met their criteria and they aimed to determine which 24-2 VF grid locations changed most rapidly and frequently in eyes with OHTN. Their findings were in agreement with previous reports on the most common locations of VF defects in early glaucoma, and while the pattern of progression was similar in both the early- and delayed-treatment groups, the rate of change and frequency of events were higher in the delayed-medication group. This further supports the use of IOP-lowering therapy.
“Supported by previous observations regarding the areas of vulnerability, our results suggest that providing hypotensive treatment to slow down the rate of glaucoma progression, might be more effective in the vulnerability zones, at least at the early stages of the disease,” the authors stated. But they cautioned, “While our findings indicate that IOP lowering mainly reduces the rate of progression in the vulnerability zones, the exact relationship between baseline IOP, the degree of IOP lowering, and patterns of progression need to be clarified and warrant further investigation.”
Authors also noted the fact that all subjects in the original Ocular Hypertension Treatment Study received treatment, either early or delayed, which could differ from the natural history of the disease. “The slopes found in the trend-based analysis might not be purely due to glaucomatous damage from OHTN and might also be affected to a certain degree by normal, age-related decline in VF pointwise sensitivity,” they said. “However, as the age-related changes are expected to be homogenous throughout the VF, this should not influence the points that would be found most vulnerable.”
They concluded, “While further studies are needed to validate these findings and evaluate their clinical significance, it seems that it might be prudent to carefully monitor [the nasal and paracentral regions] to facilitate early detection of progression and that timely treatment may help reduce the rate of progression in these locations.”
Leshno A, Bommakanti N, De Moraes CG, Gordon MO, Kass MA, Cioffi GA, Liebmann JM. Visual field progression patterns in the ocular hypertension treatment study correspond to vulnerability regions of the disc. Eye (Lond). February 14, 2024. [Epub ahead of print.] |


