 |
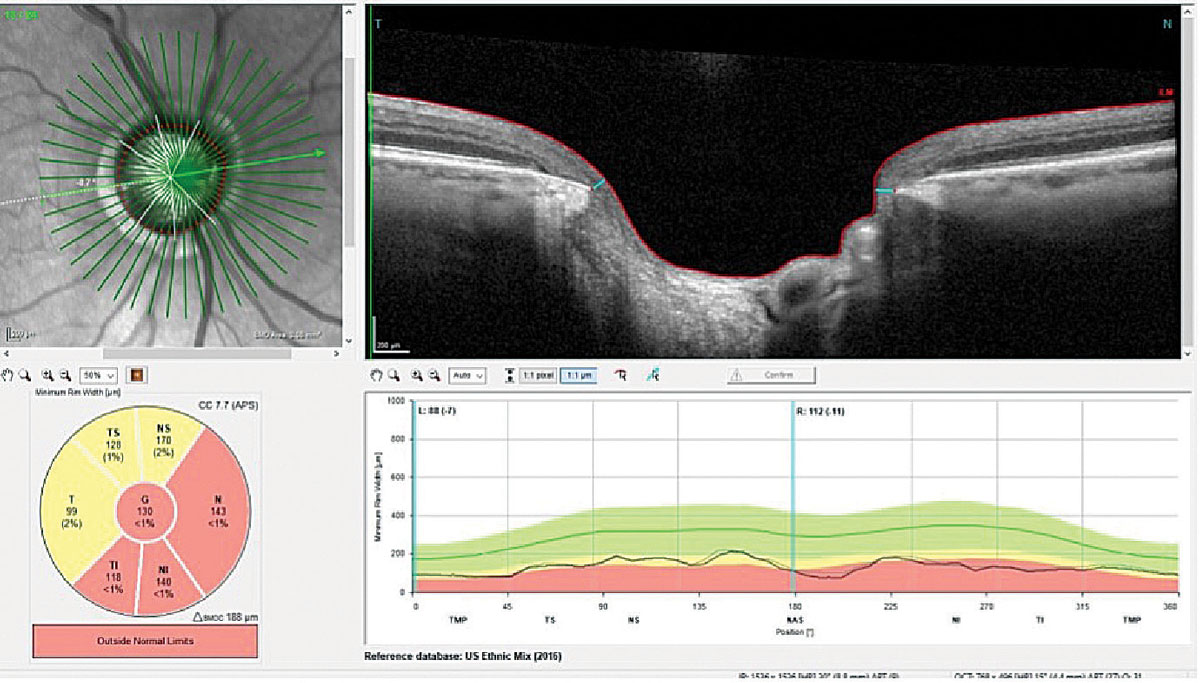
| Eyes with optic disc microvasculature dropout had significantly lower optic disc vessel density than those without, while there were no significant differences in parapapillary deep-layer vessel density between the two groups (image is from a different glaucoma patient than those studied). Photo: James L. Fanelli, OD. Click image to enlarge. |
A recent study based in South Korea hypothesized that optic disc microvasculature damage also develops in eyes with pre-perimetric glaucoma and that clinical features of eyes with optic disc microvasculature dropout differ from those without optic disc microvasculature dropout. After investigating the relationship of optic disc microvasculature dropout with disease severity (i.e., with RNFL thickness and visual field (VF) parameters), the researchers found that optic disc microvasculature dropout and lower optic disc vessel density were related to worse VF MD and thinner RNFL.
The study, published in Journal of Glaucoma, categorized 139 eyes of pre-perimetric primary open-angle glaucoma (POAG) patients according to the presence of optic disc microvasculature dropout with OCT-A. Factors including visual field (VF) mean deviation (MD), RNFL thickness, focal lamina cribrosa defect, optic disc hemorrhage and parapapillary deep-layer microvasculature dropout were compared between eyes with and without optic disc microvasculature dropout.
The researchers observed optic disc microvasculature dropout in 69 pre-perimetric glaucoma eyes (49.6%). Compared with eyes without optic disc microvasculature dropout, the ones with dropout had a significantly thinner RNFL in all areas except the nasal sector, worse VF MD and a focal lamina cribrosa defect and parapapillary deep-layer microvasculature dropout: male sex also was more highly prevalent (59.4% of those with dropout). A considerable number of eyes with optic disc microvasculature dropout lacked focal lamina cribrosa defect (62.3%) or parapapillary deep-layer microvasculature dropout (71.0%), while a few eyes without optic disc microvasculature dropout had focal lamina cribrosa defect (10.0%) or parapapillary deep-layer microvasculature dropout (2.9%).
In a multivariable logistic regression analysis, male gender (odds ratio; OR: 3.96), worse VF MD (OR: 1.44), thinner global RNFL (OR: 1.13), higher prevalence of focal lamina cribrosa defect (OR: 3.71) and parapapillary deep-layer microvasculature dropout (OR: 7.85) were significantly associated with optic disc microvasculature dropout.
“These findings suggest that impaired optic disc circulation as reflected by optic disc microvasculature dropout may be a characteristic sign of early glaucoma without noticeable changes in VF, lamina cribrosa or parapapillary deep-layer circulation,” the researchers wrote in their paper. “A possible explanation for the discrepancy is that optic disc vasculature damage precedes lamina cribrosa and parapapillary choroidal circulation alteration in the early disease phase; such changes develop subsequently as glaucoma progresses.”
The team noted that longitudinal studies are needed to elucidate whether impaired deep optic nerve head circulation plays a causative role in the development and progression of glaucoma.
Suh MH, Weinreb RN, Zangwill LM. Optic Disc Microvasculature Dropout in Pre-perimetric Glaucoma. J Glaucoma. April 16, 2024. [Epub ahead of print]. |


