 |
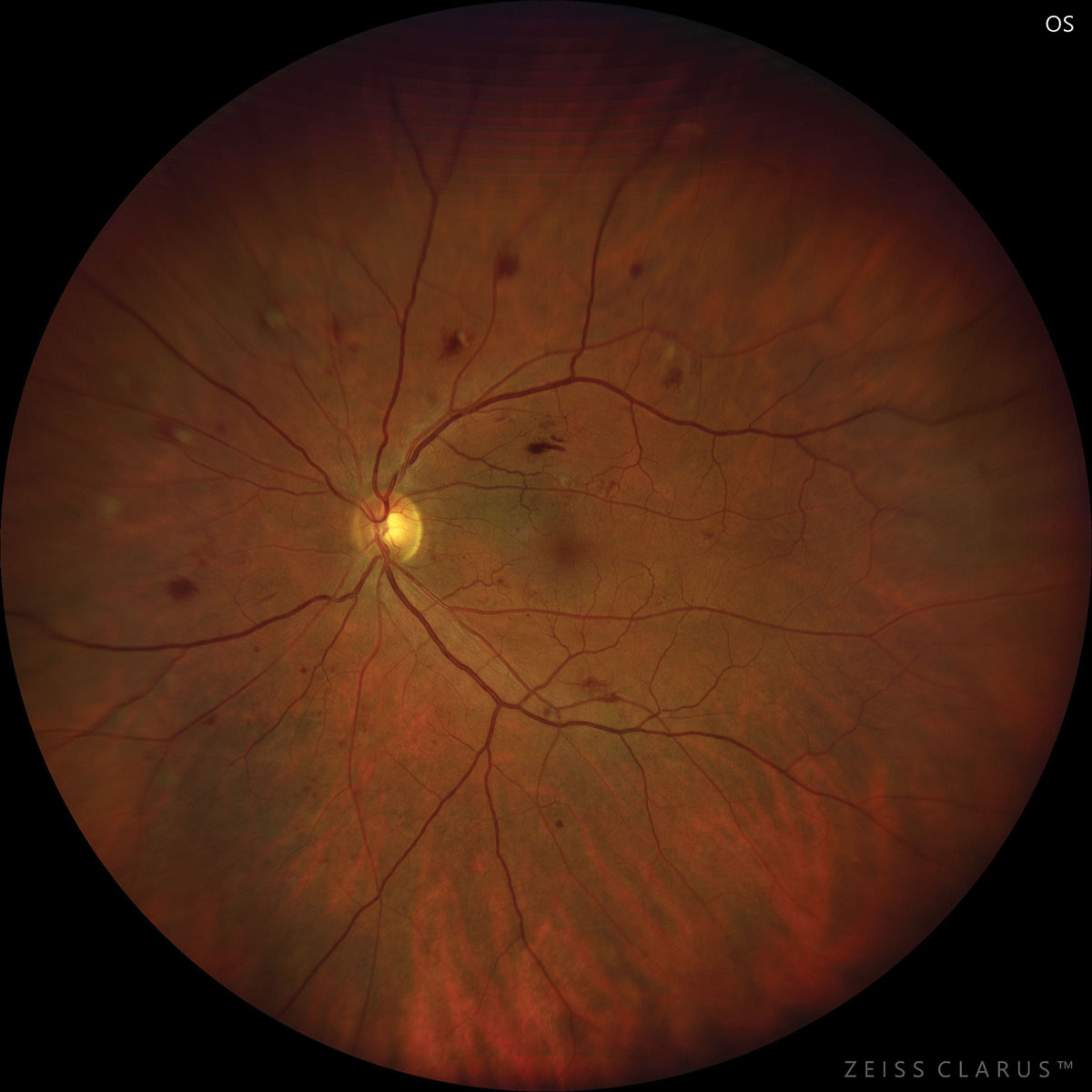
| The researchers propose that chronic hyperglycemia in diabetes patients leads to the atrophy of choroidal arterioles, causing choroidal thinning. Photo: Jay Haynie, OD. Click image to enlarge. |
Given the severity of possible ocular complication of diabetes—vision loss, macular edema, vitreous hemorrhage and retinal detachment among others—clinical methods of early identification are critical. As such, researchers of one new Retina paper wanted to investigate any associations between choroidal alterations and the reduction of peripapillary retinal nerve fiber layer (pRNFL) thickness in patients with diabetes without diabetic retinopathy (non-diabetic retinopathy, NDR).
Included in the retrospective investigation were 143 total eyes from 83 NDR patients, as well as 124 control eyes from 82 individuals. Ultra-widefield swept-source OCT angiography measured retinal and choroidal thickness, retinal vascular density and choroidal vascular metrics. The study researchers found that NDR patients displayed significant reductions in perifoveal choroidal thickness, a decrease in choroidal vascular index and an increase in choroidal stromal index. The average pRNFL thickness, outer nuclear layer (ONL) thickness and total retina all decreased in NDR patients as well. After multivariate model analysis, total choroidal thickness was correlated with pRNFL thickness, even after adjusting for confounding factors of age, sex, disease duration, HbA1c, serum creatinine, axial length and hypertension.
The authors further elaborate on their findings in the paper’s discussion. As they explain, a decrease of about 20um was found in NDR patients’ choroidal thickness, suggesting this has already decreased in these patients before substantial alterations are observed in retinal perfusion. Since the choroid mainly consists of vessels, choroidal thickness reduction, to a degree, signifies decrease in choroidal perfusion.
Total retinal thickness and ONL thickness changes were also observed. To explain these observations, the authors specify that the ONL is less directly impacted by high glucose levels and more likely influenced by choroidal perfusion due to vessel absence in this structure. Consequently, the authors posit that “a decrease in choroidal perfusion could impact the structure and function of the retina, particularly the ONL where photoreceptor nuclei are located.” The observed decrease in ONL thickness could be from photoreceptor cell apoptosis following this decreased choroidal perfusion.
Further specified is that significant thinning of the pRNFL was seen in the superior, nasal and inferior sectors, while the temporal sector showed no changes. The researchers add that another neurodegenerative eye disease, glaucoma, also displays the temporal pRNFL as the best-preserved sector. Due to the findings regarding choroidal thickness, the authors believe that “a decrease in pRNFL thickness may serve as an indicator of early retinal neurodegeneration.”
In their paper, they explain the connection and what this might mean for future investigations. “Given that the choroid supplies most of the oxygen and nutrients required by the outer retinal layers,” they wrote, “we propose a hypothesis: chronic hyperglycemia leads to the atrophy of choroidal arterioles, causing thinning of choroidal thickness. This may result in hypoxia of retinal cell nuclei located in the ONL and INL layers, affecting structures downstream in the visual transmission pathway, such as the RNFL, leading to retinal neurodegeneration.”
Li Z, Yang F, Deng X, et al. Associations between choroidal alterations and early neurodegeneration in diabetes without diabetic retinopathy: insights from ultra-widefield OCTA imaging. Retina. April 4, 2024. [Epub ahead of print]. |


