 |
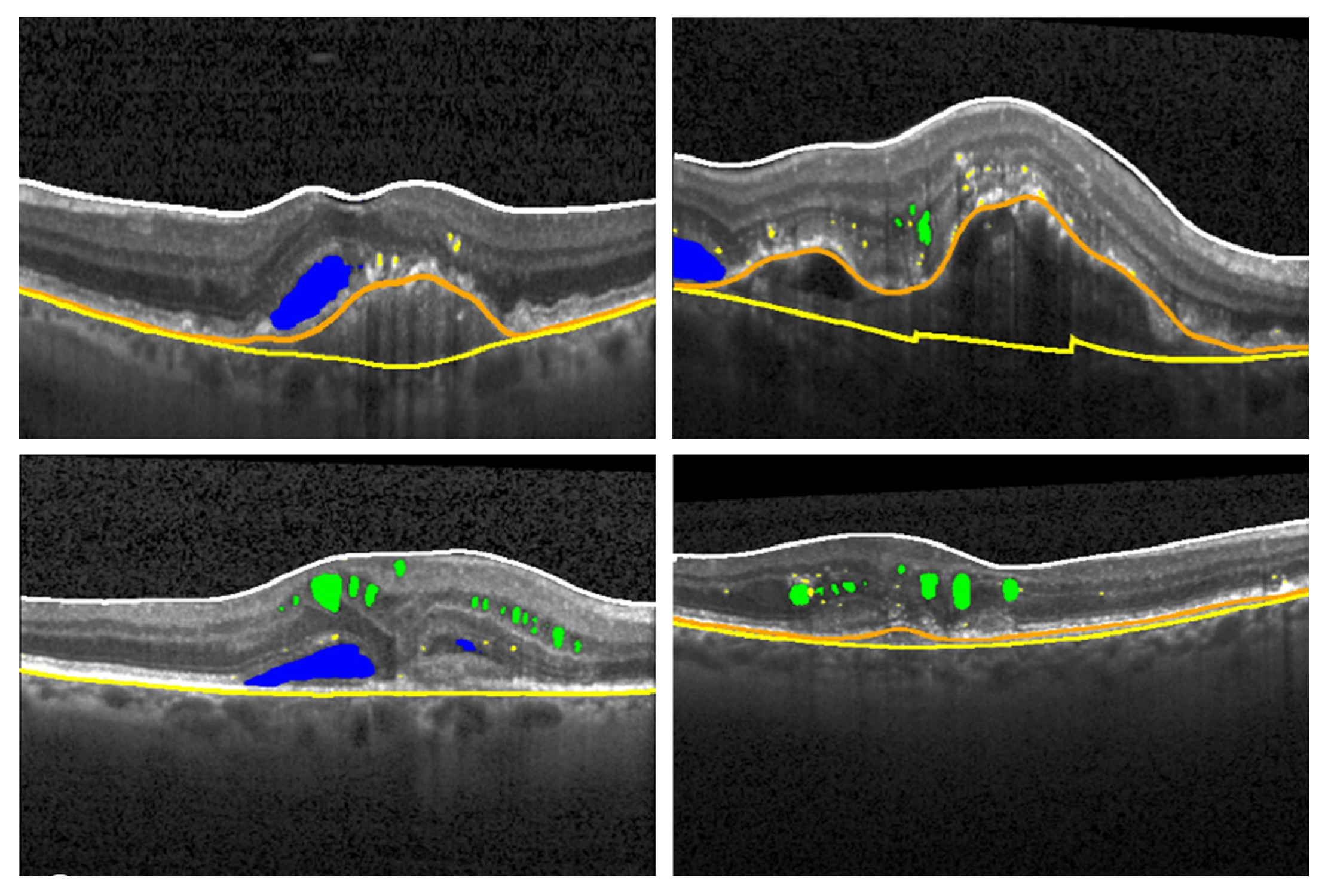
Top row: non-polypoidal MNV1, polypoidal MNV1. Bottom row: MNV2, MNV3. The researchers used AI tools to isolate fluid biomarkers in each MNV form as follows: • Cystic intraretinal fluid = green • subretinal fluid = blue • hyperreflective foci = yellow • pigment epithelial detachment = orange line • Bruch's membrane = yellow line • retinal thickness = ILM (white line) to RPE (orange line) Photo: Najeeb BH, et al. Am J Ophthalmol. Feb. 28, 2024. Click image to enlarge. |
Exudation is common in macular neovascularization (MNV) but it has many different characteristics, potentially manifesting as cystoid intraretinal fluid (IRF), subretinal fluid (SRF), pigment epithelial detachment (PED) or some combination of all three. Other relevant variables include hyperreflective foci (HRF) and retinal thickness (RT).
In addition, MNV has three potential forms:
- MNV type 1: sub-RPE “occult” choroidal neovascular membrane
- MNV type 2: “classic” subretinal membrane above the RPE
- MNV type 3: retinal angiomatous proliferation
“Each type and subtype has special exudative characteristics which influence the clinical manifestation, visual function and response to treatment,” wrote a team of researchers from Vienna in a recent paper they published in American Journal of Ophthalmology. Such variations “should be considered to optimize the management of nAMD, in particular in MNV type 3 (MNV3), which shows a unique pathological and clinical picture.”
To that end, the researchers compared the volumes and regional distribution of the five main exudative biomarkers among the MNV types and subtypes using assistance from AI in hopes of correlating findings with disease categories. The results suggest that subretinal fluid (SRF) is of choroidal origin in MNV1 while intraretinal fluid, hyperreflective foci and retinal thickness are biomarkers of retinal origin in MNV3.
The analysis included 34,528 OCT B-scans of 281 MNV3, 55 MNV2 and 121 MNV1 treatment-naïve eyes. The average volumes of cystic intraretinal fluid, subretinal fluid, pigment epithelial detachments (PED) and hyperreflective foci volumes as well as retinal thickness were compared among MNV types and subtypes.
Data showed that MNV3 cases had the highest correlation with IRF, retinal thickness and hyperreflective foci while those with MNV1 showed the greatest mean SRF. By contrast, subretinal fluid was lowest in MNV3 patients. The polypoidal subtype, when compared to non-polypoidal forms, had greater average subretinal fluid.
When considering location, the investigators found that IRF was confined to the macular center while SRF was more scattered in all types. Additionally, they observed that SRF, HRF and PED were more distributed in the temporal macular half in MNV3 presentations.
“Contrary to the current trend, where all MNV types are pooled in neovascular AMD clinical trials, this pioneer AI-based analysis shows the significancy of differences in exudative biomarkers across the known types and subtypes of MNV,” the study authors wrote in their paper.
“Cystoid IRF, HRF and RT are highly influenced by retinal neovascularization (MNV3), and SRF is rather a biomarker for choroidal neovascularization (MNV1 and 2),” they concluded. “Thus, classification of MNV is an important step for personalized medicine in neovascular AMD research, as it helps in making decisions free from a selection bias related to the MNV type or subtype.”
Najeeb BH, Gerendas BS, Deak GG, et al. An automated comparative analysis of the exudative biomarkers in neovascular age-related macular degeneration, The RAP Study: Report 6. Am J Ophthalmol. February 28, 2024 [Epub ahead of print]. |


