 |
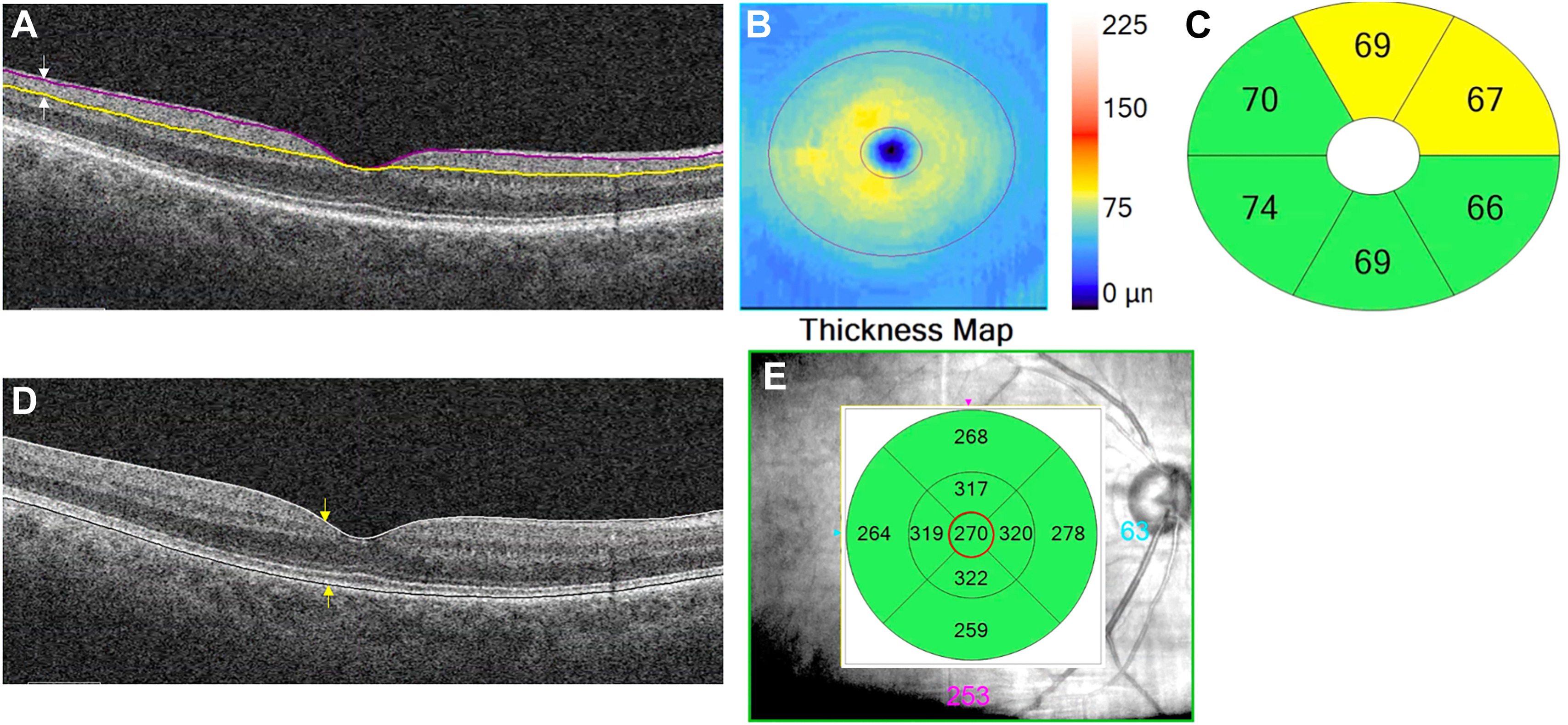
| At time of PD diagnosis, generally 50% of dopaminergic input from the substantia nigra to the striatum is lost, which might reflect the dopaminergic state of the retina. This study found small but notable differences in IPL thickness among Parkinson’s patients. (Image from a different study of retinal changes in PD.) Photo: Kundu A, et al. Ophthalmol Sci. 2023:3(4). |
Optometrists and ophthalmologists are increasingly aware that some neurodegenerative conditions—most notably Parkinson’s disease (PD) and Alzheimer’s—can cause ocular changes visible on retinal imaging. OCT studies of the retina in PD have indicated reduced thickness, which is also a key characteristic of glaucoma. One group of researchers was interested in identifying the presence and pattern of retinal changes in de novo, treatment-naïve PD patients compared with healthy controls and early primary open-angle glaucoma (POAG) patients.
To test this, macular OCT data was obtained from three cohorts of patients: 100 controls, 121 PD patients and 78 POAG patients. The Parkinson’s patients displayed a significantly reduced thickness of the inner plexiform layer and RPE compared with controls. Glaucoma patients experienced a significantly thinner RNFL, ganglion cell layer, inner and outer plexiform layers and outer photoreceptor and subretinal virtual space compared with PD patients. The only layers that were thinner in PD compared with POAG were the outer segment layer and RPE.
In their article on the work for Journal of Parkinson’s Disease, the researchers noted that the reduced thickness of these two layers in PD patients could be due to a loss of amacrine cell dendrites, possibly indicating a loss of amacrine cell bodies. The reduced inner plexiform layer thickness is in line with two previous studies, but those ones also found reduced thickness of the retinal nerve fiber layer, which was not observed in this study.
However, the observed inner plexiform layer thinning was small, making it, as the authors say, “less likely to become a future biomarker for PD.” They also explain that the de novo status of these PD patients may contribute to the lack of RNFL thinning seen in previous reports, potentially indicating this occurs later in disease progression.
POAG patients displayed much thinner retinas compared with PD patients, along with showing more diffuse pathology, affecting several retinal cell layers. POAG patients also saw a greater magnitude of thinning, with more extensive damage than PD patients.
Further explaining their findings, the researchers add that the inner plexiform layer contains neurotransmitters of dopamine, GABA and acetylcholine, as well as others, that play a pivotal role in PD. A lack of dopaminergic input in this layer may be contributing to the changes in thickness seen.
In the article, the authors relay the most important takeaways from their work: “De novo, treatment-naïve PD patients have a distinct retinal signature with reduction of especially the inner plexiform layer thickness, compared to healthy controls.” This reduced thickness “is also significantly different from early POAG patients, which suggests a possibly distinct pattern of retinal thinning in de novo PD patients.” This possible distinction should be given attention by both clinicians and researchers.
Chrysou A, Heikka T, van der Zee S, et al. Reduced thickness of the retina in de novo Parkinson’s disease shows a distinct pattern, different from glaucoma. J Parkinsons Dis. March 21, 2024. [Epub ahead of print]. |


