 |
|
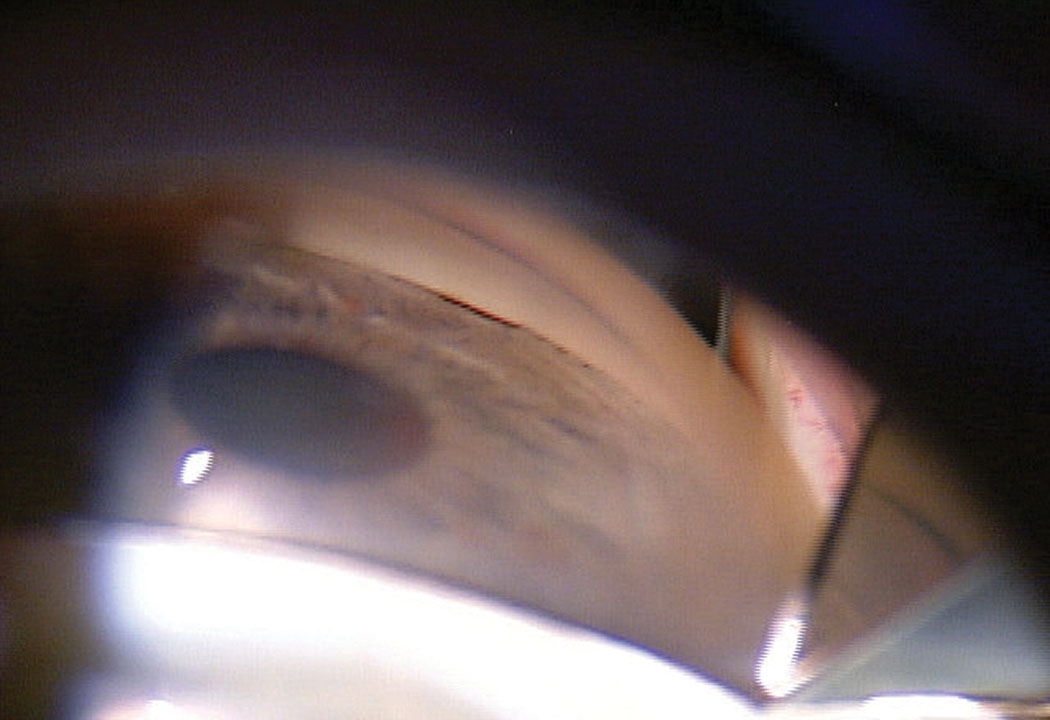
Researchers noted in their study that performing phaco surgery for primary angle closure glaucoma has its risks, since the anterior chamber is shallow and there is a lack of muscle tone in the pupil. However, their findings along with the trials reviewed in this study have supported the safety and efficacy of phaco over laser peripheral iridotomy. Photo: Michael Cymbor, OD. Click image to enlarge. |
Individuals with anatomically narrow angles are at an increased risk of angle closure glaucoma and warrant extra attention from their eye doctors to reduce chances of vision loss. Common forms of treatment include phacoemulsification and lens extraction or laser peripheral iridotomy (LPI). To better understand the difference in treatment efficacy between phaco and iridotomy procedures, researchers from Saudi Arabi conducted a systematic review and meta-analysis study.
In order to provide the best possible results, researchers excluded randomized controlled trials that did not include a comparison or phacoemulsification and laser peripheral iridotomy. Furthermore, if studies did not measure outcomes such as prevalence of rising intraocular pressure, number of glaucoma medications taken throughout treatment, Shaffer gonioscopy grading, visual acuity, visual field, central endothelial cell density, central corneal thickness, peripheral anterior synechiae and poor responses to treatment, these studies were eliminated from the review. Five studies with a total enrollment of 917 patients (455 phaco subjects; 462 LPI subjects) were accepted for this review.
“The analysis showed statistically significant lower central corneal thickness, central endothelial cell density and risk of poor response to surgery in phacoemulsification compared to laser peripheral iridotomy,” reported the researchers in their study. “On the other hand, no significant differences in intraocular pressure, number of medication usage, visual field, peripheral anterior synechiae, mean Shaffer gonioscopy grading and visual acuity.”
This review has its limitations. For instance, each trial that was examined for this review provided results with various follow-up periods. Due to the time variations, the researchers were not able to properly compare intraocular pressure at different points. Additionally, the analyzed follow-up periods lacked longevity. Only one randomized controlled trial followed up with their subjects over a 10-year period. Other limitations cited by the researchers were an absence of data on cost comparisons and the inclusion of studies written solely in English.
Despite these limitations, the researchers explained that the observed trials demonstrated a low rate of heterogeneity. Now, knowing the effectiveness between phacoemulsification and laser peripheral iridotomy, physicians can make more conscious decisions on which treatment to recommend for primary angle closure glaucoma.
Sharif RK, Aljahdali FF, Aljabri HM, et al. Phacoemulsification versus laser peripheral iridotomy for treating primary angle closure glaucoma: a systematic review and meta-analysis. Clinical Ophthalmology. 2024;18:1023-32. |


