 |
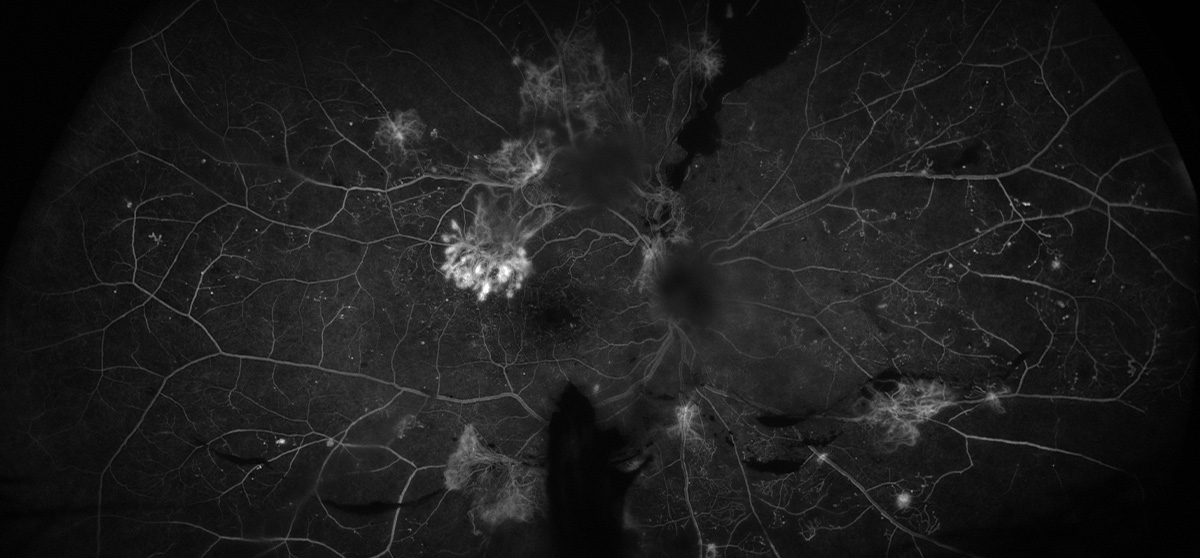
| Researchers analyzed parameters such as hyperlipidemia, total cholesterol levels and intraocular pressure and found that results differed significantly based on the presence or absence of carotid stenosis. Photo: Rami Aboumourad, OD. Click image to enlarge. |
New research conducted in Korea explores the interconnectedness of proliferative diabetic retinopathy (PDR) and internal carotid artery (ICA) stenosis. “Atherosclerosis, accelerated by diabetes, contributes to arterial narrowing in both carotid and retinal vessels, exacerbating ischemic changes in the retina and advancing PDR progression,” the researchers point out in their paper on the work.
In their analysis, the researchers studied 68 diabetic retinopathy patients (136 eyes). Each patient was assessed for carotid artery stenosis using neck CT angiography and carotid duplex ultrasound. This allowed the researchers to categorize their subjects into two groups: normal (Group 1) and mild or above (Group 2). Then they used OCT and OCT angiography to measure retinal parameters such as subfoveal choroidal thickness, retinal nerve fiber layer (RNFL) thickness, ganglion cell-inner plexiform layer thickness, vessel density and foveal avascular zone area.
A total of 51 patients (102 eyes) were placed in Group 1 and 17 (34 eyes) in Group 2. There was a statistically significant difference in total vessel density, foveal avascular zone area, total retinal nerve fiber layer thickness, and temporal RNFL thickness between the two groups that showed significant thinning in Group 2 with severe carotid artery stenosis. There was no significant difference in subfoveal choroidal thickness, central vessel density, average ganglion cell-inner plexiform layer thickness, and superior, nasal and inferior RNFL thickness.
“These alterations underscore the necessity for carotid artery evaluation in proliferative diabetic retinopathy patients, suggesting a link between internal carotid artery stenosis, blood flow changes, and retinal health,” noted the researchers in their study. “Monitoring RNFL thickness could be vital for assessing vascular health and risk in patients with carotid artery stenosis, offering a potential biomarker for early intervention to prevent cerebrovascular events.”
Although the researchers’ results further linked carotid stenosis to PDR, this study had its limitations. Due to the small sample size, the researchers were limited to a cross-sectional retrospective design, which made it difficult for them to confirm changes in RNFL thickness. Also, they failed to compare changes in carotid artery stenosis when RNFL defects were not observed.
“Despite some limitations, these findings emphasize the need for further research to establish the role of retinal nerve fiber layer thickness in managing and improving outcomes for patients with carotid artery stenosis,” stated the researchers in their journal article.
Lee CY, Park JM, Yeom MI. Risk factors of internal carotid artery stenosis in patients with proliferative diabetic retinopathy: An analysis using optical coherence tomography and optical coherence tomography angiography. BMC Ophthalmology. 2024;24(1):156. |


