 |
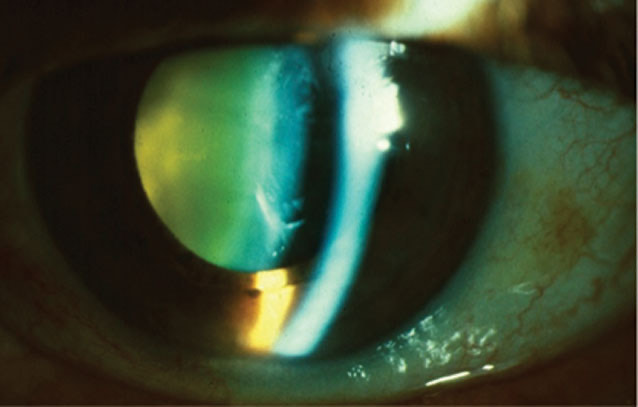
| Cataracts increase a patient’s risk of vascular mortality. Photo: Julie Tyler, OD. Click image to enlarge. |
Patients with cataracts may face up to a 36% increased risk of vascular mortality, according to a new study published in the British Journal of Ophthalmology. The investigation also found a positive association between self-reported cataract surgery and all-cause mortality based on a large-scale, population-centered sample.
A total of 14,918 participants were included in the study’s analysis of National Health and Nutrition Examination Survey data from 1999 to 2008. A self-reported history of cataract surgery was considered a surrogate for the presence of clinically significant cataract surgery, and mortality data were verified from National Death Index records. After roughly 10 years, approximately 19% of the participants had died.
Overall, the researchers found that individuals with self-reported cataract surgery were more likely to die from all causes and specific causes (vascular disease, cancer, accident, Alzheimer’s disease, respiratory disease, renal disease and others) compared with individuals without cataract. Still, no significant association was observed specifically between self-reported cataract surgery and cancer, respiratory disease, renal disease, Alzheimer’s disease, accidents or other cause-related mortality.
There have been a few hypotheses explaining the association between cataract and vascular mortality, including oxidative stress, which has been implicated in the pathogenesis of both cataract and atherosclerosis, the study authors noted. Additionally, previous studies of human lens epithelial cells found that the senescence of lens cells, triggered by oxidative stress-induced DNA damage and telomere shortening, contributed to cataract formation.
Oxidative stress affects vascular reactivity, and oxidized low-density lipoproteins promote atherogenesis, and therefore, the presence of cataract may be an indicator of high levels of cumulative oxidative damage resulting from physiological and pathological aging, the researchers explained.
Another alternative hypothesis is that crystallins are also involved in regulating apoptosis, cell survival and responses to stressors such as inflammation and ischemia, not only at an ocular level but also at a systemic level, they added.
The authors also found that participants in their study who had a history of bilateral cataract surgery were more than twice as likely to die from renal disease. A plausible mechanism linking cataract and renal disease-related mortality could be increased oxidative stress, which is implicated in both cataracts and chronic kidney disease, the investigators said.
Chen Y, Wang W, Liao H, et al. Self-reported cataract surgery and 10-year all-cause and cause-specific mortality: findings from the National Health and Nutrition Examination Survey. Br J Ophthalmol. October 25, 2021. [Epub ahead of print]. |


