 |
|
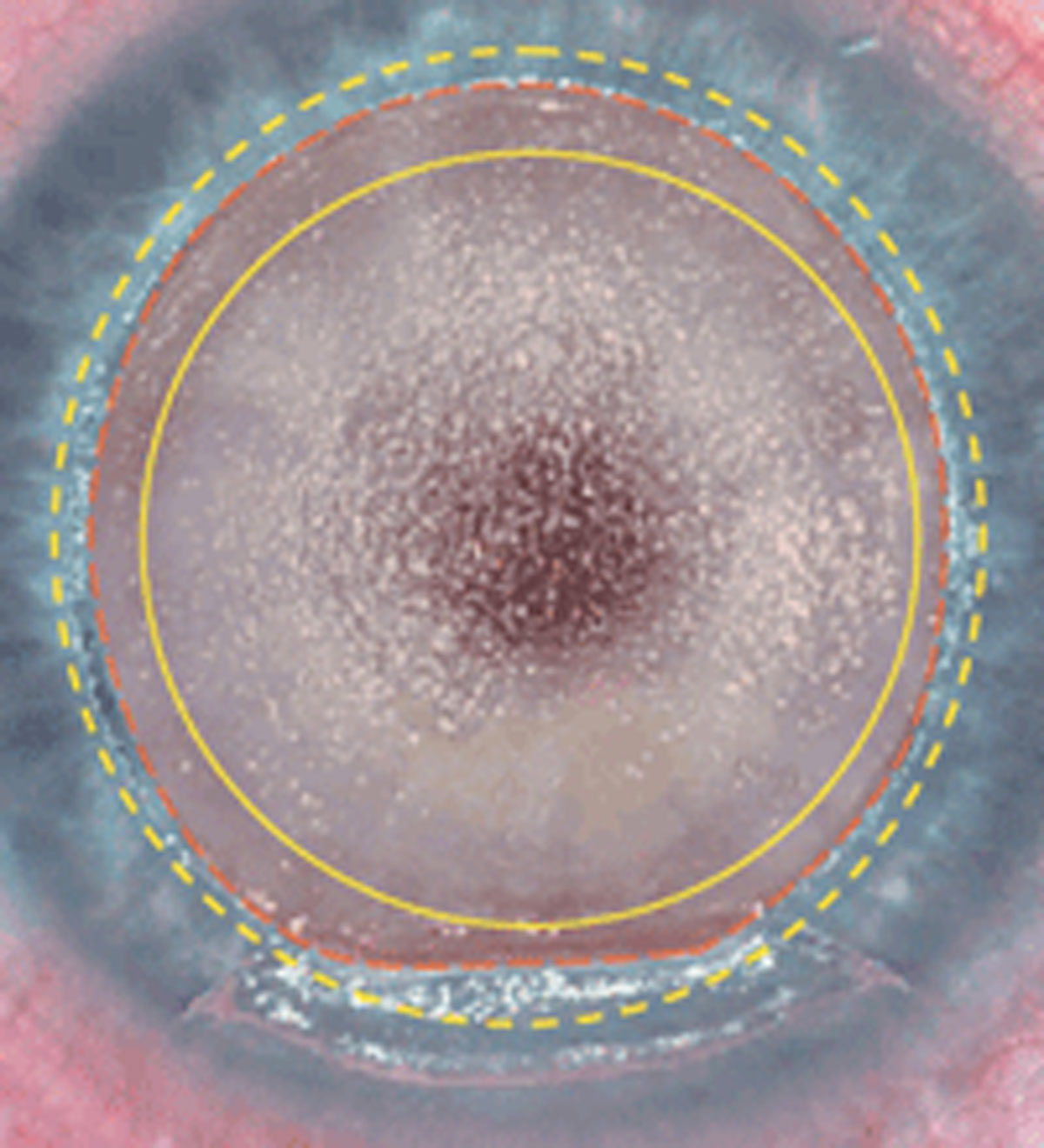
LASIK reduces dendritic cell density in the central cornea, creating a stimulus for cellular migration to the area. These changes may manifest clinically as ocular surface disruption and pain long after the surgery. Photo: Martin L. Fox, MD. Click image to enlarge. |
While LASIK can significantly improve a patient’s quality of life, it does also expose individuals to certain complications or unintended effects, one being corneal nerve damage during flap creation. What are its consequences? One new study examines LASIK’s effect on corneal epithelial dendritic cell (CEDC) density as well as morphology. It additionally outlines the relationships of corneal nerves and tear neuropeptides.
“LASIK disrupts corneal immune homeostasis by reducing the number of resident immune cells in the cornea and by changing the morphology and hence role of those cells. We believe this change is associated with nerve damage,” says Fiona Stapleton, PhD, FCOptom, and Cecelia Chao, PhD, FCOptom, both of the School of Optometry and Vision Science UNSW Sydney and members of the research team conducting the study. “Nerve damage after LASIK disrupts the close communication between the immune system and the nerves, which can lead to chronic neurogenic inflammation and result in eye pain.”
The prospective study—including 20 LASIK patients and 20 controls—examined in vivo confocal microscope images of the central cornea; the post-LASIK participants had received the surgery 12 to 16 months prior. The density of CEDCs was manually counted and a new grading system was used in assessment of morphology. “This is very exciting as we can now apply this to different diseases, trauma or other challenges to the ocular surface and better understand how the eye responds,” Drs. Stapleton and Chao say.
Results showed that post-LASIK participants displayed lower dendritic cell density at the central cornea in comparison with controls. Postsurgical patients also displayed an almost threefold higher proportion of CEDCs with thicker dendrites than controls, and more total dendrites. Even further, a higher tear substance P concentration corresponded with both a higher CEDC density and an absence of long dendrites. Participants with CEDCs that had dendrites displayed fewer nerve connections. The more numerous and thicker dendrites observed in post-LASIK participants is thought to be due to an enhanced migratory capacity of the cells.
This study provides additional evidence that LASIK can disrupt the corneal neuro-immune crosstalk important in homeostasis and increase chronic neurogenic inflammation. “Optometrists should have a degree of suspicion that postoperative patients may be at risk of neurogenic inflammation and discomfort due to LASIK, even if they were asymptomatic before the procedure,” Drs. Stapleton and Chao advise. “They may exhibit pain without stain on examination after the procedure.”
The two researchers advise optometrists to consider appropriate diagnostic testing in such patients, including the need to test the structure and function of corneal nerves and assess for ocular surface damage and the presence of inflammation. “Appropriate strategies for managing ocular pain or neuropathic corneal pain should be offered to these patients” as well, they say.
Chao C, Tajbakhsh Z, Stapleton F, et al. Corneal epithelial dendritic cells, tear neuropeptides and corneal nerves continue to be affected more than 12 months after LASIK. Acta Ophthalmol. 2022. [Epub ahead of print]. |


