 |
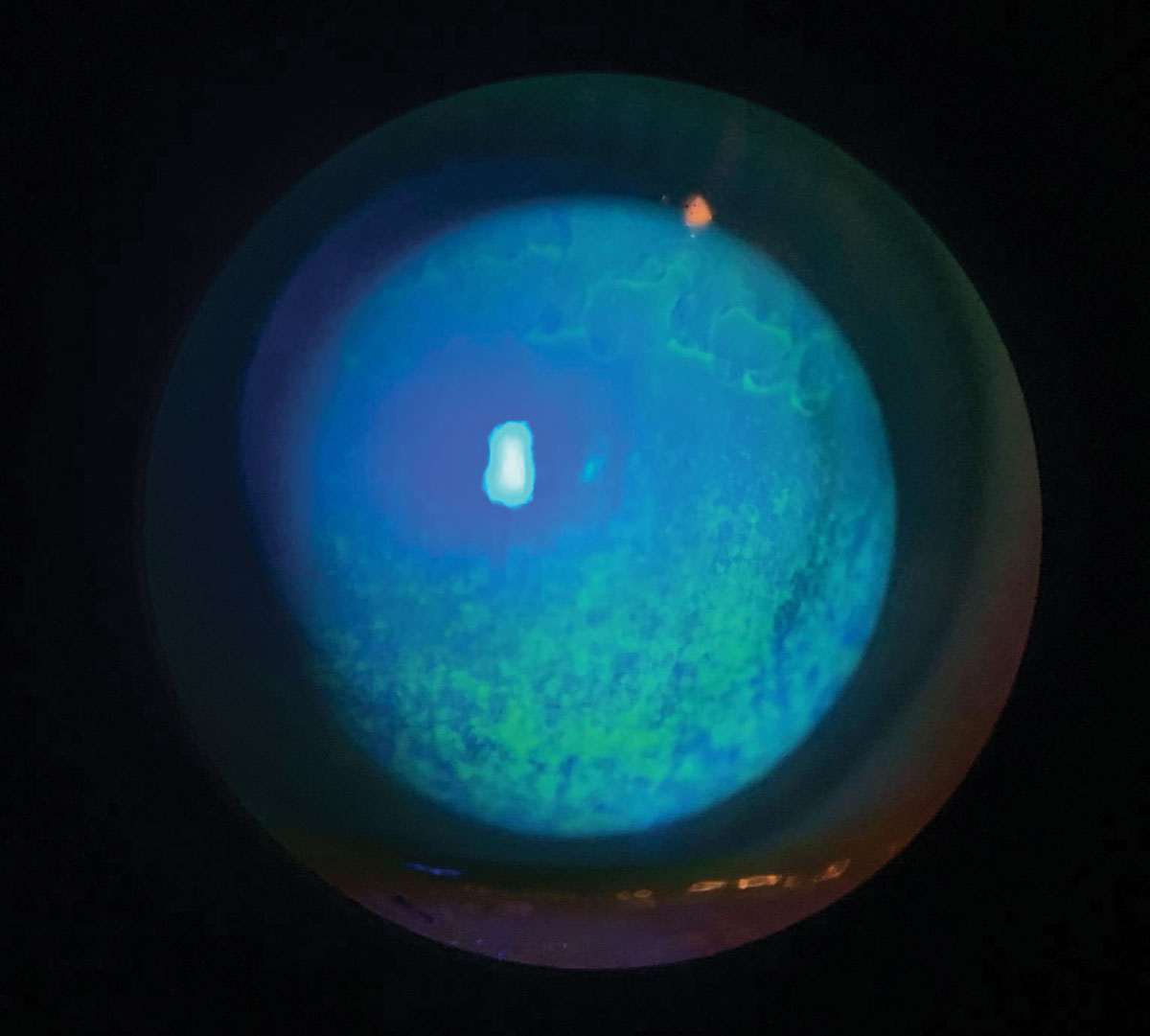
| Patients with preexisting DED are more likely to experience tear film instability post-upper blepharoplasty. Photo: Candice Tolud, OD. Click image to enlarge. |
Damage to the ocular surface following upper blepharoplasty can contribute to the development of postoperative complications such as dry eye. A new study looking into this correlation found patients with pre-existing dry eye had more dramatic tear film instability and worse symptoms six months after the procedure, while individuals without the condition experienced mild changes that resolved within three months postoperatively.
The research team from China enrolled 20 patients (19 females and one male) between the ages of 21 and 35 who underwent upper blepharoplasty at the Eye, Ear, Nose and Throat Hospital of Fudan University.
Twenty-one eyes of 11 participants had no pre-existing dry eye symptoms compared with 18 eyes of nine subjects who had DED. All participants underwent testing preoperatively and again at one, three and six months after the surgery. Testing included OSDI questionnaires, Schirmer 1, tear meniscus height, lipid layer thickness, noninvasive tear breakup time (NITBUT), fluorescein tear film breakup time (FBUT), corneal fluorescein staining, meibum expression, lid margin changes and tear inflammatory cytokine evaluation.
For DED patients, their OSDI scores increased significantly at one month but then decreased to baseline levels at six months. DED participants also had significantly shortened first NITBUT and FBUT readings at all follow-ups. On the other hand, individuals without dry eye symptoms at baseline only had shorter first NITBUT and FBUT readings at one month, but these measures returned to preop levels by six months.
Considering tear inflammatory cytokines, the researchers noted an increase of interleukin (IL)-6 in both groups, while IL-8 and tumor necrosis factor alpha (TNF-α) were only higher in individuals who had DED postoperatively. Additionally, IL-8 and TNF-α levels were positively correlated with OSDI scores, but they didn’t appear to be linked with first NITBUT and FBUT measures.
Since pre-existing dry eye may be a larger risk factor for worse and persistent ocular surface damage following the procedure, surgeons should complete a preoperative assessment, recognize preoperative dry eye and address rational medication use such as artificial tears and topical anti-inflammatory agents prior to surgery, the investigators suggested.
To improve preoperative assessment, elevated inflammatory cytokines might be a more sensitive marker for the development of dry eye than traditional parameters, especially in those with separated symptoms and signs, the authors added.
Zhao S, Song N, Gong L. Changes of dry eye related markers and tear Inflammatory cytokines after upper blepharoplasty. Front Med. December 9, 2021. [Epub ahead of print]. |


