 |
|
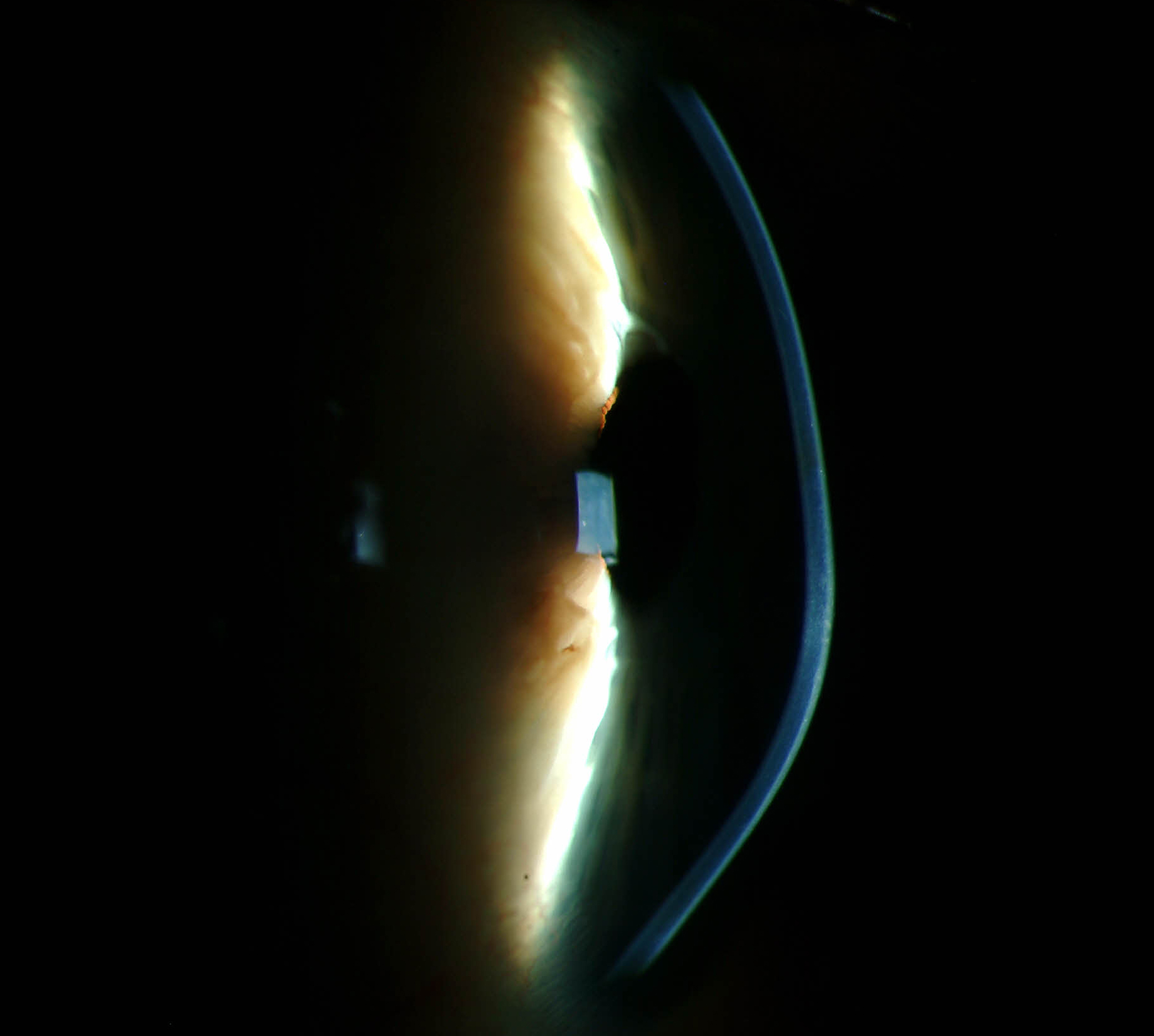
Keratoconus in those who did rub their eyes was related to high frequency of rubbing, but not the intensity or duration. Click image to enlarge. |
While factors that are associated with keratoconus have been established, new research found additional factors that have not yet been outlined. The prospective, single-center study was comprised of case and control groups of 195 patients each, matched one to one from each group for age and sex. The case group included patients who had keratoconus in at least one eye and had followed up with a corneal specialist and controls displayed no evidence of keratoconus upon a slit-lamp exam and corneal topography.
The researchers collected patient data via self-completed questionnaires. Upon review of the results, they found significant associations of the condition with a family history, eye rubbing, allergies of any kind, smoking history and dry eyes. They also found a positive correlation between disease severity and extent of eye rubbing as well as night-time pressure due to sleep position. The role that pressure plays on the eye when sleeping, as well as smoke exposure and dry eyes, comprise the list of lesser known risk factors.
Looking more closely at the factor of eye rubbing, the researchers found additional associations that better elucidate why this becomes such a problem. Most importantly, the eye that patients preferentially rubbed was the worse eye. Keratoconus in those who did rub their eyes was related to high frequency of rubbing, but not the intensity or duration.
The part of the hand used to rub the eye was significant as well, as rubbing using knuckles or the back of the hand was associated with keratoconus and the case group used the index fingertip to rub the eye less than the control group. Since the case group used harder parts of the hand, their eyes were subsequently exposed to more mechanical power through bone contact.
The researchers contend that the reason smoke exposure was found as a factor is because it would result in dryness and likely rubbing of the eye. They also propose different hypotheses for this association, including the notion that meibomian gland dysfunction and dryness due to smoke may increase friction. Another possible explanation: personality may contribute to increased eye rubbing in those with higher anxiety.
While the authors did find the most significant risk factors of development to be family history, allergy, and eye rubbing, they advise practitioners to pay attention to one of the novel factors found—sleep position. They propose “all patients should be systematically screened for inappropriate sleeping positions to identify the use of nighttime eye protection if necessary.” They also touch on how to approach the most important factor, eye rubbing, since it is fairly easy to prevent. They are optimistic that “helping people to stop eye rubbing could be an effective treatment on its own to stop the progression of ectasia. In addition, it can be a target for primary prevention by educating the population to not adopt these behaviors.”
Debourdeau E, Planells G, Chamard C, et al. New keratoconus risk factors: a cross-sectional case—control study. J Ophthalmol. September 28, 2022. [Epub ahead of print]. |


