 |
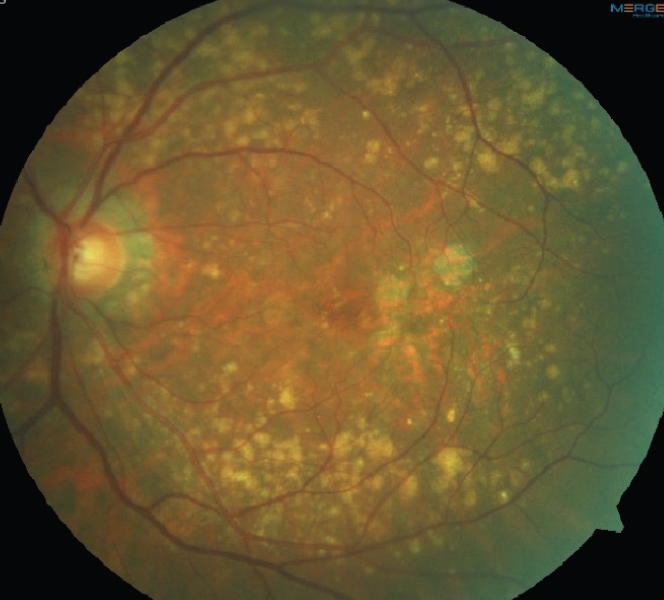
| Clinical signs like drusen arise from lipid dysfunction and have different systemic associations than subretinal drusenoid deposits or other lipid-derived entities. Photo: Anna Bedwell, OD. Click image to enlarge. |
Though lipid and cholesterol dyshomeostasis is thought to contribute to the pathogenesis of age-related macular degeneration (AMD), there is no consensus regarding which elements of systemic lipid levels are perturbed in AMD. In a new systematic review and meta-analysis, an update to one performed in 2016, researchers characterized serum lipoprotein profiles in patients with AMD and its various stages. They found that there is significant heterogeneity in systemic lipoproteins in patients with AMD, and the specific pattern of lipid dyshomeostasis appeared to be distinct based on AMD stage.
This meta-analysis included 58 studies and 308,188 patients, almost three times as many compared with the 2016 meta-analysis, which had included 19 studies and 104,270 patients. Included articles reported blood/serum levels of lipid subspecies (triglycerides, total cholesterol, low-density lipoprotein [LDL] and high-density lipoprotein [HDL]) in patients with AMD compared with controls.
When analyzing all AMD patients regardless of stage of disease, the team found no differences in any of the lipid subspecies compared with controls. On the other hand, when analyzing patients with early to intermediate AMD separately, there were significantly lower levels of triglycerides and higher levels of HDL but no differences in the levels of total cholesterol or LDL. Patients with advanced dry AMD had no significant differences in triglycerides, total cholesterol, LDL or HDL. Patients with advanced wet AMD had significantly higher systemic LDL but no differences in triglycerides, total cholesterol or HDL.
“Taken together, our results highlight the significant heterogeneity of AMD and suggest that the specific aspects of lipid homeostasis that are perturbed may depend on the underlying stage or subtype of disease,” the authors wrote in their paper for Ophthalmology Science.
They noted that these findings may explain, in part, why there is a discrepancy in the literature published to date with respect to the specific facets of lipid function and dysfunction that are associated with the pathophysiology of AMD.
“We speculate that among patients with AMD, there may be facets of lipid dyshomeostasis that are specific to certain stages of the disease process,” the article explained. “In fact, recent studies have shown that patients with soft drusen are distinct from those with subretinal drusenoid deposits (SDDs) on the basis of their systemic associations, serum profiles and genetic risk profiles and provided evidence that high HDL was associated with classic soft drusen, whereas low HDL was associated with SDDs.” These prior studies also found an association between SDDs and coexisting systemic vascular disease (e.g., aortic stenosis, myocardial infarction) and suggest that both low HDL and presence of SDDs may be related to systemic atherosclerosis.
“We propose that these findings reflect the underlying heterogeneity of AMD, the presence of distinct pathophysiological mechanisms involved at different stages of AMD and may even suggest the existence of distinct AMD subtypes that should be investigated further to inform novel therapeutic approaches,” the authors concluded.
Li B, Goss D, Miller JW, et al. Systemic dyslipidemia in age-related macular degeneration: an updated systematic review and meta-analysis. Ophthalmol Sci. May 24, 2023. [Epub ahead of print]. |


