 |
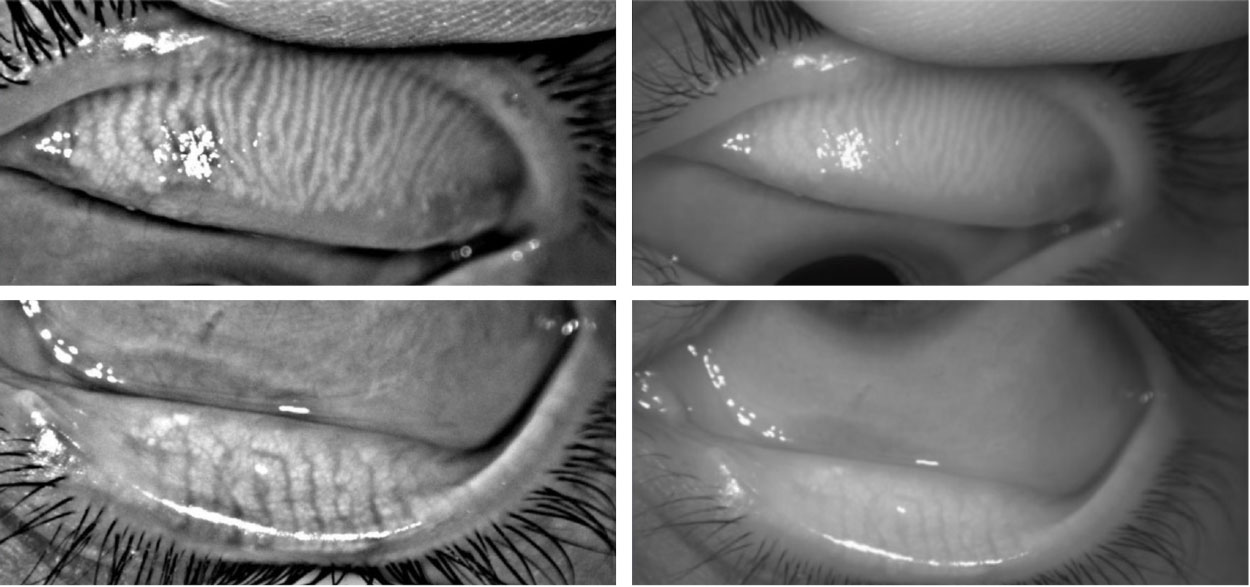
| Images captured with anterior segment OCT showed significantly greater meibomian gland length than those captured with standard meibography (shown), suggesting that optimized wavelength devices could provide better information about how patients respond to dry eye disease treatment. Photo: Katherine Sanford, OD. |
It’s generally believed that a person’s fully functioning meibomian glands begin to atrophy permanently due to age and other factors, contributing to dry eye disease (DED). The process is somewhat reversible, as some studies have shown an increase in visible meibomian glands and their improved function after thermal pulsation treatment, suggesting that the glands are revitalizing/regrowing. Given the importance of accurate gland assessment in dry eye management, a new study questions whether the meibomian glands are being fully captured by current meibography devices.
Researchers compared upper and lower eyelid images taken with the traditional Keratograph 5M at a wavelength of 880nm to the Visante OCT at a wavelength of 1,310nm to determine if a deeper visualization into the eyelid revealed more meibomian gland length. Thirty asymptomatic patients with normal tear films were analyzed. Meiboscores based on K5M and the Visante OCT were significantly different for the lower eyelid (0 vs. 1) but not the upper eyelid (0 vs. 0). The mean gland visibility percentages of upper eyelid (82.7% vs. 75.2%) and lower eyelid (81.2% vs. 64.1%) were significantly greater on the Visante OCT than K5M images, respectively. This suggests that traditional meibography imaging may be missing viable segments of the meibomian glands and overrepresenting the amount of gland atrophy after DED therapy.
The authors hypothesize that the discrepancy between the upper and lower eyelid scores could be attributed to the “natural slight thickening of the lower eyelid palpebral conjunctiva compared to the upper eyelid.” Where it has been generally accepted to only examine the lower tarsus in cases of meibomian gland atrophy, this study further underscores the impact of using OCT to evaluate these cases, they continued.
In their paper for Contact Lens and Anterior Eye, the study authors state that OCT’s decreased contrast sensitivity compared to the K5M did lose some of the finer details of the images, but had little impact on the overall benefits of using the technology. “In our current study as a preliminary indication, we have established that OCT can detect a greater meibomian gland visibility compared to meibography,” said the authors. “This result suggests that traditional meibographers may overlook a significant portion of the meibomian glands in normal, asymptomatic participants.”
Another point made in the study is how to characterize meibomian gland morphology changes. The authors say current subjective meibomian gland grading uses coarse scales, such as 0, 1, 2 and 3 corresponding to 0%, 1-<33%, 33-67% and >67% amounts of atrophy. The current study used ImageJ, which is a freely available analysis tool able to quantify MG length changes down to the percent, and this method was able to find significant between-method differences,” they stated. “Thus, these data suggest that if clinicians are aiming to use meibography to track disease progression, they should grade percent gland lost rather than with integer scales. While typically not a feature on commercially available meibography devices, this grading method could be easily incorporated by manufacturers.”
Among the primary limitations of the study was the absence of DED or a clinically meaningful amount of meibomian gland atrophy among participants. “This study design approach was taken because the primary goal was to determine if there were between-machine differences in being able to image visible meibomian gland length,” explained the authors. “This study should be repeated in a larger group of participants with and without DED who are longitudinally evaluated to determine if OCT images of the meibomian glands are affected by treatment and to determine if imaging differences between participants with and without DED are present.”
Based on these results, clinicians should consider using meibography devices with optimized wavelengths to ensure capturing a full picture of their patients’ meibomian gland health.
Ravichandran S, Pucker AD. Comparing meibomian gland visibility on optical coherence tomography and Keratograph 5M images using objective and subjective grading methods. Cont Lens Anterior Eye. April 1, 2024. [Epub ahead of print]. |


