 |
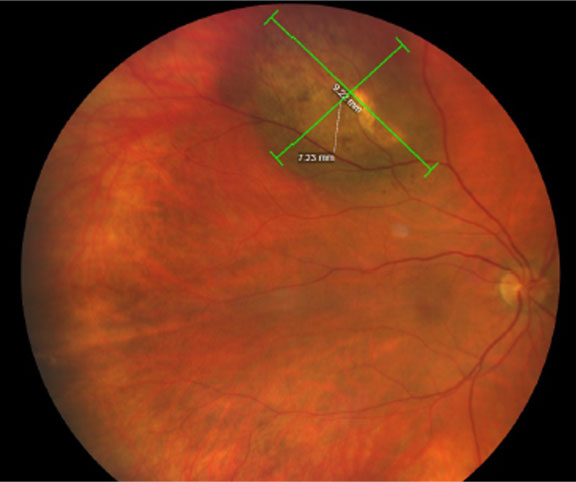
What’s known as ‘the obesity paradox’ could apply in uveal melanoma, as those who were obese had a lower risk of developing metastases and consequently dying than those with lower BMIs. Photo: Amy Bade, OD. Click image to enlarge. |
Only 2% of patients with uveal melanoma have clinical metastases at diagnosis. Research has shown, however, that early on in the disease, micrometastases may have developed in distant organs, where they can remain dormant for years. This explains the concerning 60% survival rate at 20 years.
Body mass index (BMI) is a good indicator of metabolic status and may play into a person’s risk of metastasis development or proliferation. Obesity has been observed to cause systemic inflammation and contribute to the development and progression of breast cancer. Nutrient deprivation may also activate autophagy in dormant cancer cells.
Considering prior research that shows how a higher BMI can negatively affect certain types of cancer, the results of a new study may surprise you. Its data showed that obesity and elevated serum leptin levels—which closely correlate to an increase in body fat—are actually associated with a lower risk for developing metastases and dying from uveal melanoma.
The study included 683 patients diagnosed with uveal melanoma between 2009 and 2017 at an average age of 64 years; all cases were diagnosed and cared for at an eye hospital in Stockholm. Twenty percent were obese, and 1% had metastatic disease at presentation. Before the end of the follow-up period, 144 passed away from metastatic disease and 114 from other causes. Of the surviving participants, the average follow-up was 6.3 years.
The researchers noted in their paper that “tumor diameter, type 2 diabetes and use of insulin were associated with metastases, but patients with obesity had a lower risk.” They reported that the incidence of melanoma-related mortality was also significantly lower for patients with obesity. Five and 10 years after diagnosis, the mortality incidence was 9.9% and 11.3% for patients with obesity and 20.3% and 24.6% for patients without obesity.
Above-average serum leptin levels were also associated with a reduced risk for metastasis, independent of sex and cancer stage. Additionally, the researchers noted in their paper for British Journal of Ophthalmology that “tumors with BAP1 mutation and epithelioid cells had higher leptin receptor RNA expression levels, which have a negative correlation with serum leptin levels.”
To make sense of these findings, the researchers provide a hypothesis. “The prognostic implication of obesity in uveal melanoma may be related to elevated serum leptin levels, which suppresses tumor leptin receptor expression, in turn reducing the activity of pathways that are associated with vasculogenic mimicry, extracellular matrix interactions and invasive behavior,” they wrote. They also pointed out that similar beneficial effects of high serum leptin levels have been found in other cancers including pancreatic cancer, colorectal carcinoma and cutaneous melanoma.
“As observations of the beneficial implication of obesity and high leptin levels are seemingly contradictory to the general notion that obesity is a poor prognostic factor in cancer, the term ‘the obesity paradox’ has been transferred to cancer after being coined in a study of the beneficial influence of BMI on mortality in patients on hemodialysis,” the researchers noted in their paper. “Herein, we have shown that this concept can be transferred to uveal melanoma.”
The researchers advise that further research will be needed to better understand the underlying mechanisms behind the association between obesity and metastasis risk.
Sabazade S, Opalko A, Herrspiegel C, et al. Obesity paradox in uveal melanoma: high body mass index is associated with low metastatic risk. Br J Ophthalmol. April 7, 2023. [Epub ahead of print]. |


