 |
|
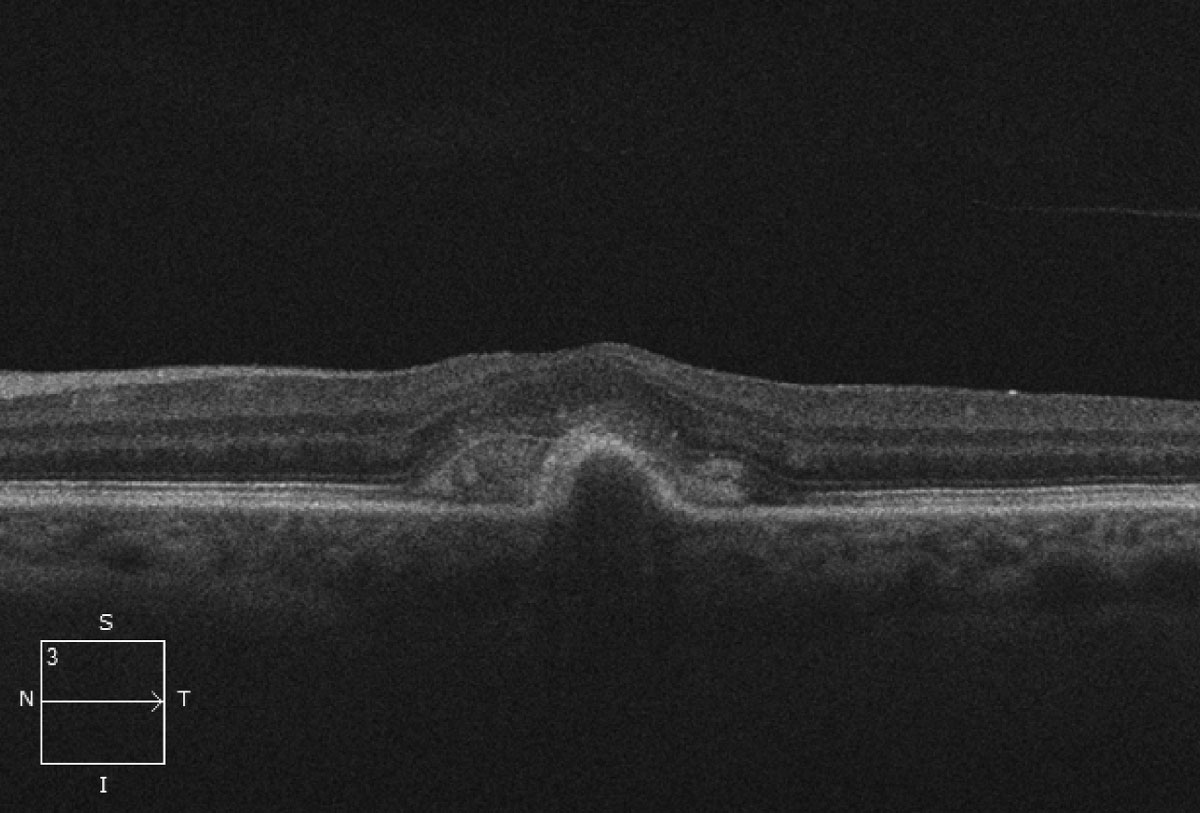
PED volume could predict the short- and long-term BCVA gains for non-PCV after intravitreal injection of conbercept. Photo: Mark T. Dunbar, OD. Click image to enlarge. |
In this study, researchers determined the predictive value of quantitative morphological parameters for pigment epithelial detachment (PED) of neovascular age-related macular degeneration (nAMD) patients. The results showed that intravitreal conbercept therapy of three injections pro-re-nata (PRN) could effectively improve the BCVA in patients.
One eye from each of 159 patients with nAMD were studied and split into two groups: 77 with polypoidal choroidal vasculopathy (PCV) and 82 without. They received conbercept 0.05mL (0.5mg) in a three-injection PRN treatment regimen. Correlations between retinal morphologic parameters at baseline and best-corrected visual acuity (BCVA) gain at three or 12 months after treatment (structure-function correlations) were assessed. OCT scans were used to assess retinal morphologic features including intraretinal cystoid fluid, subretinal fluid, PED or PED type and vitreomacular adhesion. Greatest height, width and volume of PED at baseline were also measured.
The results are similar with previous studies that suggested PED had a negative correlation with BCVA gain for non-PCV, which could be due to the association of PED with choroidal neovascularization, where larger neovascularization was associated with poorer prognosis for vision. “The volume also better reflects the scope and extent of the lesion, which we found to have markedly different influences on BCVA gain,” the authors noted.
It also showed that wider PED at baseline correlates to less BCVA gain at 12 months. “This is most likely due to retinal structure damage caused by the extent of the lesion, which may depend on the duration of the pathology,” the authors explained.
A wider PED translated to larger and more severe lesion. In the short-term, through active treatment, BCVA may see improvement yielding no significant negative correlation between BCVA gain and PED width.
“Following disease progresses, some other retinal structural damage, such as atrophy of the RPE may emerge, thus the favorable results observed at three months after treatment may not be able to be maintained in the long term, resulting in a poorer prognosis,” they noted.
The BCVA gain in three or 12 months in the non-PCV group was greater than that in the PCV group, although there was no significant difference. PED volume at baseline in PCV group was larger than that in non-PCV group, while BCVA gain was relatively smaller, although there was no statistical difference between the two groups, which may explain why PED has an indication effect for non-PCV group but not for PCV group, the authors suggested. They do not believe that PED volume at baseline may still affect vision prognosis.
“PED is not a good evaluation of the visual prognosis for patients with PCV, as it may be related to bleeding and serous fluid,” they wrote in their paper. “After absorption, the vision prognosis may be more positive.”
Shu Y, Ye F, Liu H, et al. Predictive value of pigment epithelial detachment markers for visual acuity outcomes in neovascular age-related macular degeneration. BMC Ophthalmology. March 3, 2023. [Epub ahead of print.] |


