 |
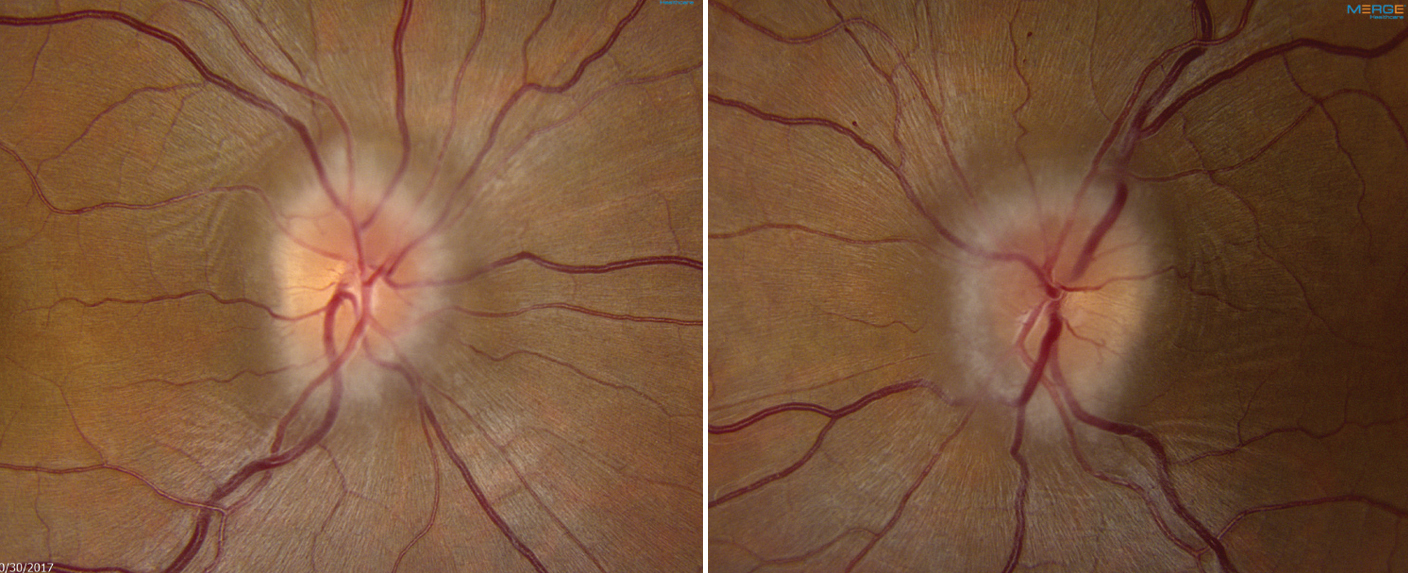
| Previous studies reporting up to 57% of IIH cases include comorbid PCOS may have overestimated, based on this study’s findings. Photo: Mark Dunbar, OD. Click image to enlarge. |
Editor’s Note: As part of our “Year in Review” retrospective, we’ve selected the top 30 news stories of the year and are re-sharing them as we close out 2023. Follow along as we count down to number 1!
This story was originally published May 25, 2023.
No. 17 biggest news story of 2023:
Both manifestations of idiopathic intracranial hypertension (IIH) and polycystic ovary syndrome (PCOS) are hyperandrogenic metabolic disorders, highlighting the need to determine how the two may be connected. Furthering the need for a concrete association is the fact that the reported prevalence of comorbid PCOS with IIH is highly variable.
Included in the study were 398 women with IIH and documented PCOS. Questionnaires were given, and patients were followed for a median of 10 months. The comorbid prevalence was determined to be somewhat high at 20% (n=78) using Rotterdam criteria for diagnosis. This percentage dropped to 9% when using NIH criteria. The current literature estimates 15% by NIH criteria.
Fertility problems were self-reported to be higher among IIH patients with comorbid PCOS, representing a 3.2-fold increased risk, while increased need for medical help in becoming pregnant was associated with a 4.4-fold increased risk. However, PCOS comorbidity did not adversely impact headache outcomes or long-term vision. Along with this finding, headache burden was high in both cohorts.
The study authors point out that both IIH and PCOS have been linked with decreased fertility, with this study showing that any dual pathology of the two conditions may result in further increased fertility difficulties. Although the causes of this increased difficulty are likely multifactorial, the researchers hypothesize that hyperandrogenism, insulin resistance and obesity are plausible contributors, all of which are common to both conditions.
It is important to call attention to resolved papilledema demonstrating recovery over time with IIH. Obesity is common in both conditions, but this study demonstrated similar baseline BMIs in IIH patients with PCOS and those without, suggesting that PCOS does not exacerbate any phenotypic obesity seen with IIH. However, weight loss is the only disease-modifying therapy currently for IIH, which can reduce papilledema and intracranial pressure. Weight loss similarly would benefit those with PCOS, especially with the addition of metformin in comorbid patients to enhance weight loss.
Looking at the instances of headache in this study, the researchers found morbidity to be high and predominantly migraine-like characteristically. Although the researchers hypothesized coexistent PCOS to exacerbate migraine headaches with IHH, this was not found to be the case. Instead, headache morbidity was high in the entire cohort. This is important to note as severe headaches with IIH can continue after papilledema and intracranial pressure resolve. Cases like these have shown promising results with CGRP monoclonal antibody therapies administration.
“Our results have implications for clinical practice as they suggest that those with IIH should have PCOS identified as they may benefit from gynecological or endocrinological specialist management,” the team concluded in their paper for the journal Eye. “Discussing fertility with patients may also include that pregnancy does not adversely impact visual outcomes in IIH in those with well-controlled IIH at the time of conception (particularly in those who have resolved papilledema.”
Thaller M, Homer V, Sassani M, et al. Longitudinal prospective cohort study evaluating prognosis in idiopathic intracranial hypertension patients with and without comorbid polycystic ovarian syndrome. Eye. May 24, 2023. [Epub ahead of print]. |


