 |
|
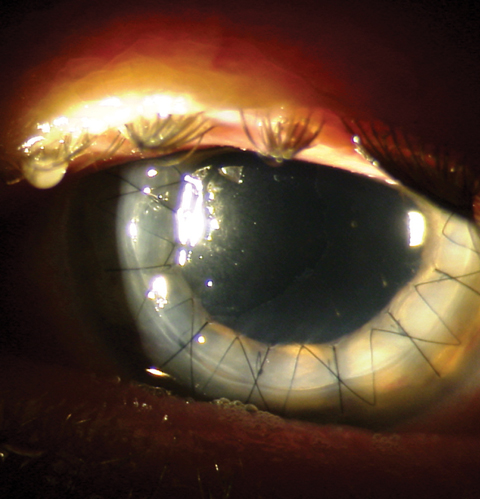
The volume of corneal transplantation for infectious keratitis has remained stable over the last decade, with the exception of Acanthamoeba-related cases. Click image to enlarge. |
While infectious keratitis may require corneal transplantation to control the infection, few studies have reported on graft survival or the role of human leukocyte antigen (HLA). The purpose of this recent study was to analyze real-world practice patterns and graft survival after corneal transplantation for infectious keratitis. It showed that viral keratitis was the most common indication for transplantation, followed by bacterial and Acanthamoeba keratitis.
A total of 1,111 keratoplasties for infectious keratitis that were registered in the Netherlands Organ Transplant Registry between 2007 and 2011 were analyzed. The most common pathogens were viruses, bacteria and Acanthamoeba.
HLA matching did not provide a significant survival benefit, whereas non-HLA-matched procedures showed worse graft survival. Most transplants were performed for visual rehabilitation (optical keratoplasty), with several focusing on debulking and preserving globe integrity (therapeutic keratoplasty).
“Lower graft survival of larger grafts in our cohort may be related to a higher antigenic load in the proximity of the limbus increasing the risk of rejection and a more severe infection requiring debulking,” the study authors wrote in their paper.
Two-year graft survival for therapeutic viral keratitis measured 77%, which is high compared with previous studies reporting 55% to 75% at two years. “The cause of failure is manifold; for instance, in herpes simplex keratitis, stromal keratitis is associated with deep vascularization, which increases rejection risk, and disease recurrence is common after nerves regenerate in the graft,” the researchers explained. “Moreover, herpes keratitis is accompanied by hypoesthesia, which facilitates recurrent trauma and exposure keratopathy. The relatively high graft survival in our cohort may be related to standard use of oral prophylaxis to prevent herpes recurrence in the Netherlands.”
Two-year graft survival of therapeutic keratoplasty for bacterial keratitis was 81%, slightly lower than that reported in previous studies (over 90%).
Two-year graft survival was 72% for therapeutic keratoplasty and was comparable between viral and bacterial keratitis but substantially lower in Acanthamoeba keratitis, even after correcting for type, reason for surgery and graft size. The volume of corneal transplantation for Acanthamoeba keratitis accounted for 14% of all indications and increased from a handful of cases before 2009 to double digits since 2015. “This increase may be due to the use of silicone hydrogel contact lenses, multipurpose solutions or local environmental factors,” the team noted. “Importantly, Acanthamoeba keratitis showed the worst outcomes of all causative agents even when outcomes were adjusted for type of procedure (HLA-matched, emergency and elective non-HLA-matched procedure), reason for grafting (optical and therapeutic keratoplasty) and graft size.”
“The benefit of HLA matching is unclear, but our data suggests that it may not provide additional survival benefits,” the investigators concluded. “Timely therapeutic keratoplasty should be considered as needed given the relatively successful outcomes in our study, especially for viral and bacterial keratitis.”
Veugen JMJ, Dunker SL, Wolffs PFG, et al. Corneal transplantation for infectious keratitis: a prospective Dutch registry study. Cornea. February 4, 2023. [Epub ahead of print]. |


