 |
|
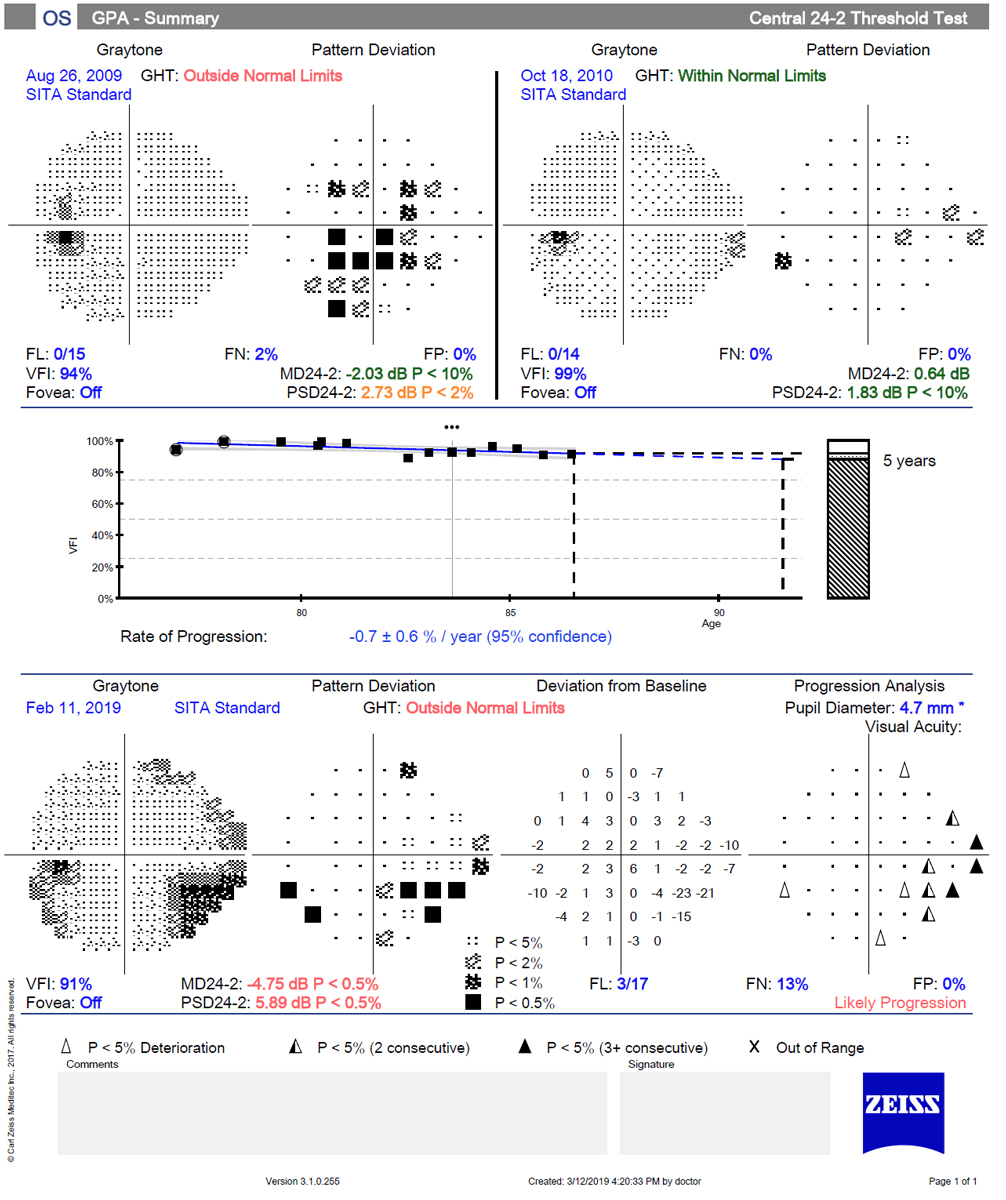
Despite the noted superior testing of the 24-2, the authors believe that the 10-2 is the test of choice for monitoring eyes with advanced damage. Photo: Danica Marrelli, OD. Click image to enlarge. |
Researchers sought to understand the differences in performance of two types common testing protocols in standard automated perimetry (SAP)—10-2 and 24-2. OCT was used as an independent standard for glaucomatous damage.
The study conducted—including 339 subjects—was cross-sectional. It examined 569 eyes and included 1,375 pairs of 10-2 and 24-2 SAP tests. A total of 77% of the eyes had diagnosed glaucoma while 23% were normal, and all participants underwent the 10-2 and 24-2 SAP tests within 30 days. To quantify glaucomatous severity, researchers used OCT macula ganglion cell layer (mGCL) and circumpapillary retinal nerve fiber layer (cpRNFL) as measures.
Findings generally resulted in better performance of the 24-2 SAP test across different stages of the disease when compared to the 10-2 test. This was especially true of earlier stages of the disease.
When considering mild macular damage, it may be thought that the 10-2 test would better pick up this type of damage. The researchers believe the 24-2 may be detecting this type of damage better than the 10-2 because significant damage may have already occurred in the periphery.
Additionally, detection of RNFL loss in both perimetric tests was more modest when looking at eyes with mild or moderate glaucomatous damage. This makes sense and reflects that it is likely much harder to detect eyes with earlier structural damage than more severe.
Looking at prior research, the authors make note that the 10-2 test may detect up to a third of macular damage that would otherwise gone unnoticed by the 24-2. Despite this seeming advantage, the studies in question reported higher central glaucomatous damage frequencies than previously. The authors believe these studies’ convenience samples to have been tested by the 10-2 SAP because of clinicians’ concern for macular damage, subsequently representing a biased sample that is not reflective of the general population of those with glaucoma.
More outside data indicates that visual fields are not carried out to the frequency recommended by professional organizations when it comes to glaucoma management. As such, the researchers posit that adding routine implementation of 10-2 visual testing on top of conventional 24-2 testing would add unnecessary strain and lack any obvious benefit. They do point out alternative ways of testing that might work better. One such is the 24-2C test, additionally including 10 test points within the central 10 degrees. This would in turn expand the central visual field sampling.
Despite the noted superior testing of the 24-2, the authors leave with a cautionary note that “the findings of this study should not be interpreted as if the 10-2 adds no value to the clinical management of glaucoma. In fact, the 10-2 test is the test of choice for monitoring eyes with advanced damage where no or little visual sensitivity is observed outside the central 5° or 10° of the central visual field.” In fact, they even think “the 10-2 test may also be useful in monitoring defects that threaten fixation.” They believe further studies are needed to determine whether it would be clinically relevant to either switch to or add 10-2 testing for glaucoma management.
Zicarelli F, Ometto G, Montesano G, et al. Objective quantification of posterior segment inflammation: measuring vitreous cells and haze using optical coherence tomography. Am J Ophthalmol. September 6, 2022. [Epub ahead of print]. |


