 |
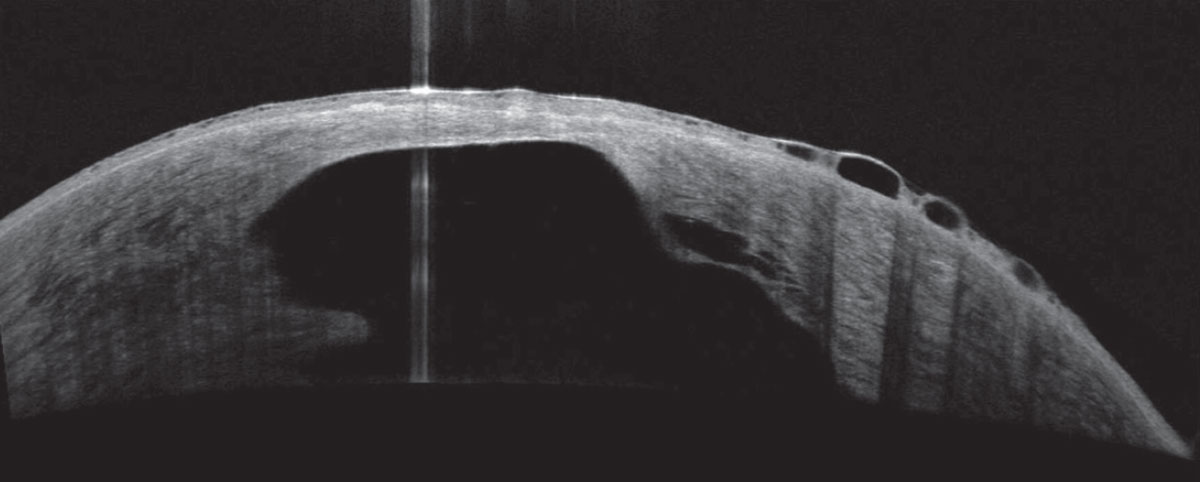
CXL patients recorded a 2.48-times greater likelihood of corneal hydrops than those managed with contact lenses. Photo: Joseph Shovlin, OD. Click image to enlarge. |
Presented Sunday at ARVO in New Orleans, a study by Cleveland-based researchers covered the lifetime prevalence of acute corneal hydrops in keratoconic eyes one year post-treatment of corneal collagen crosslinking (CXL) or contact lenses.
The retrospective study collected data from electronic health records to identify keratoconic patients and their initial treatment modality: either CXL or management with contact lenses. The primary outcome was acute corneal hydrops incidence after one year of treatment as a result of complications from continuing unstable keratoconus in spite of treatment.
Keratoconus was found in 32,141 patients. Of those, 12.1% chose to manage the condition with contact lenses, and 3.1% patients underwent CXL treatment. On average, contact lens patients were older, female and Black. Of those managed with contact lenses, 16 patients (0.4%) developed corneal hydrops one year after treatment compared with 10 CXL patients (1.0%). This culminates to an almost 2.5-times higher odds of hydrops development after CXL treatment.
The researchers determined that CXL patients possessed a higher absolute risk and likelihood of developing lifetime incidence of corneal hydrops than contact lens users. Along with this, the contact lens-managed group displayed greater event-free survival probability of hydrop acquirement over time relative to the CXL group. Additionally, the contact group had a lower hazard rate.
However, as Julie Song, OD, of SUNY College of Optometry, notes, the study’s results are somewhat misleading due to the age of each subgroup population. The patients managed with contact lenses were on average 15 years older than those in the CXL group, with average ages of 44 and 28, respectively. Keratoconic eyes tend to stabilize around age 40, she points out, which may be why hydrops prevalence was lower in the older age group. The younger CXL group was “in the age range of patients who are still susceptible to natural keratoconic progression,” which is likely a contributing factor to greater hydrops incidence, Dr. Song says. She adds that “patients who tend to undergo CXL are often patients who are already identified as having progression in their keratoconus, which is why they were referred to undergo the procedure to begin with.”
Although acute corneal hydrops is displayed here as a rare complication in both groups, the authors relay that “clinical significance remains unclear, as acute corneal hydrops represents a rare lifetime complication in both cohorts, and patients managed with CXL may be at higher risk for complications in general.” They also noted that several factors must be considered when managing keratoconus, as Dr. Song echoes, and that corneal hydrops typically spontaneously resolve within two to four months along with conservative management.
Original abstract content © Association for Research in Vision and Ophthalmology 2023.
Nguyen C, Siso D, Truong N, et al. Lifetime incidence of corneal hydrops in keratoconic eyes post corneal collagen crosslinking vs. contact lens management. ARVO 2023 annual meeting. |


