 |
|
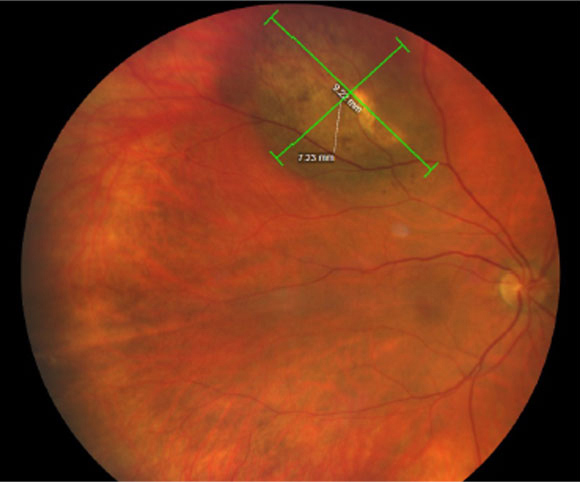
One finding from this new study was that anteriorly located tumors may increase IOP earlier on. Photo: Amy Bade, OD. Click image to enlarge. |
Tumor- or treatment-related secondary glaucoma is an extra burden to a patient with uveal melanoma. Besides any necessary medical therapy, which may be needed for a long period of time, it necessitates additional visits to the clinic. At worst, secondary glaucoma in an eye with uveal melanoma can result in painful vision and even blindness. Researchers recently noted that secondary glaucoma at initial uveal melanoma diagnosis is associated with a high risk of synchronous metastases. They have suggested that initial retinal detachment and higher intraocular pressure (IOP) with tumor thickness could inform interim assessments of IOP and neovascularization.
The study, published in Ophthalmology Glaucoma, collected patient, tumor, treatment and follow-up data from 781 patients (median age: 64) consecutively diagnosed with uveal melanoma during a 15-year period in a national ocular oncology service, 708 (91%) of whom received ruthenium (50%) or iodine (50%) brachytherapy. The team defined secondary glaucoma as an IOP ≥24mm Hg together with any of the following: (1) measured on at least three consecutive follow-up examinations, (2) considered an indication for treatment before the third examination or (3) associated with emergent anterior segment neovascularization.
The researchers determined that 45 patients (6%) had tumor-related secondary glaucoma at diagnosis, with 34 (76%) of these cases from a narrow-to-closed angle (25 had direct angle invasion) and 10 (22%) from anterior neovascularization. However, the team found that 168 patients, 165 of whom were treated with brachytherapy, developed tumor- or treatment-related secondary glaucoma a median of 1.7 years after tumor diagnosis. The cumulative proportion of developing secondary glaucoma was 23% at five years.
The most common mechanism was neovascularization in 119 patients (72%). By multivariable regression, initial retinal detachment in three to four quadrants, initial IOP of ≥17mm Hg and tumor thickness predicted incident secondary glaucoma.
Nevertheless, the research team found it reassuring that 568 patients (73%) did not develop any tumor- or treatment-related glaucoma during a median follow-up of 6.2 years.
“Secondary glaucoma can arise long after primary treatment, at a time when review for tumor control already takes place once a year,” they wrote in their paper. “Our data suggests that more frequent follow-up might still be reasonable in patients with thick tumors, initial retinal detachment and initial higher IOP.”
They noted that their data also suggests anteriorly located tumors increase IOP earlier on, reinforcing the importance of considering uveal melanoma in eyes with unilateral high IOP of unknown etiology. The iris and the anterior chamber angle should be examined carefully with gonioscopy for invasion and neovascularization related to a more posterior tumor, but other mechanisms for high IOP are also common.
Stadigh AE, Puska PM, Kivelä TT. Incidence and risk factors for secondary glaucoma in eyes with uveal melanoma. Ophthalmol Glaucoma. August 11, 2022. [Epub ahead of print]. |


