 |
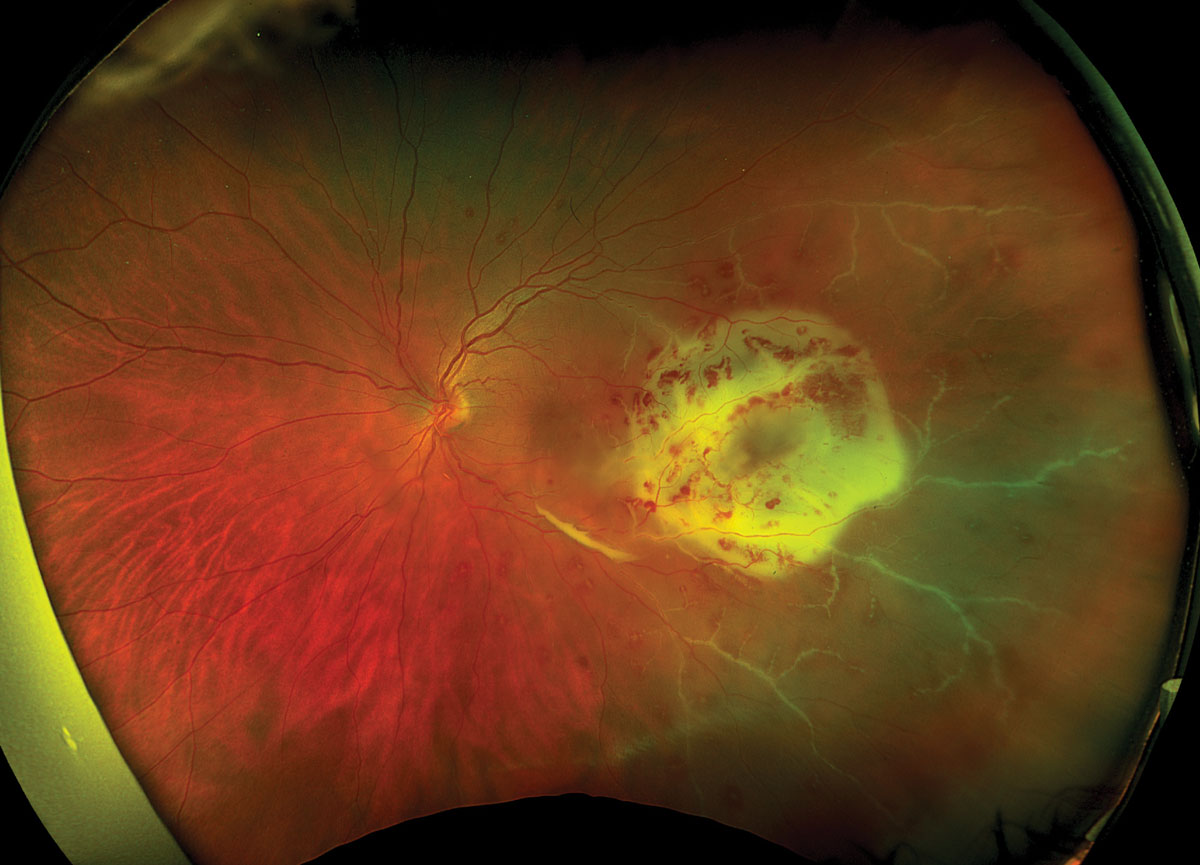
| Higher rates of vitrectomies were seen in the South and Midwest regions compared to the Northeast and West for patients presenting with endophthalmitis. Photo: Rami Aboumourad, OD. Click image to enlarge. |
Among the most visually threatening conditions in eye care, endophthalmitis typically occurs when organisms from the ocular flora of the anterior eye structures gain access to the intraocular space, chiefly during cataract surgery. A rarer form of the condition arises when a blood-borne pathogen reaches the eye in the presence of systemic infection; this is termed endogenous endophthalmitis to distinguish it from external (or exogenous) sources of infection. It has the potential for rapid progression and severe visual impairment.
Understanding regional variation in endogenous endophthalmitis is not only important for accurate diagnosis and appropriate management but also has implications for visual outcomes. Researchers at Rutgers New Jersey Medical School explored the interplay between regional variation and microbial infection in endogenous endophthalmitis and its possible impact on surgical intervention with pars plana vitrectomy (PPV) or mortality. Their findings revealed significant regional differences in patient demographics, comorbidities, microbial etiology, use of PPV and mortality rate throughout the US.
This retrospective analysis, recently published in Ophthalmology Retina, used the National Inpatient Sample (NIS) database. Endogenous endophthalmitis cases were stratified regionally into Northeast, South, West and Midwest cohorts.
A total of 10,912 patients with infectious endogenous endophthalmitis were identified, with 18.9% of cases in the Northeast, 19.7% of cases in the Midwest, 37.9% of cases in the South and 23.6% cases in the West. Analysis indicated significant regional variation in patient demographics, causative microbes, comorbidity patterns, mortality rates and surgical interventions. The most common pathogens across all regions were methicillin-sensitive Staphylococcus aureus (MSSA), Streptococcus, Candida and methicillin-resistant Staphylococcus aureus (MRSA). While MSSA was the predominant pathogen in all regions, the proportions varied significantly. Streptococcus was the second most common pathogen in the Northeast and Midwest, while MRSA held this position in the South and Candida in the West.
The Northeast had the highest proportion of in-hospital mortality, most likely as a direct result of systemic complications caused by virulent organisms. “This region also had a much higher proportion of the 80+ age group, which may have contributed to increased frailty and possibly a more complicated hospital course,” the authors noted in their paper. “This study showed an in-hospital mortality rate of 8% to 15%, depending upon region, and is generally in agreement with other studies from the US and other developed nations.”
The South and Midwest regions had higher rates of PPV for endogenous endophthalmitis, which also might suggest a regional variation in practice pattern.
“Understanding and addressing regional variations may expedite optimal diagnosis, management, and outcome of endogenous endophthalmitis,” the study concluded. “Tailored treatment strategies, informed by regional microbial patterns, may lead to improved empirical therapy and better visual outcomes. Efforts should be directed towards reducing regional outcome disparities through improved access to specialized ophthalmic care, early diagnosis and prompt initiation of appropriate treatment.”
Aftab OM, Dupaguntla A, Khan H, et al. Regional variation of infectious agents causing inpatient endogenous endophthalmitis in the US: a national analysis. Ophthalmol Retina. March 14, 2024. [Epub ahead of print]. |


