 |
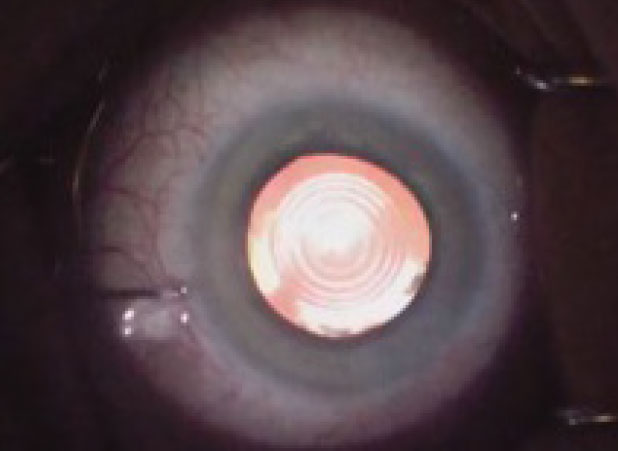
| Intraoperative aspects can also influence IOL performance, such as size and centration of the capsulorhexis. Photo: Katherine Rachon, OD. Click image to enlarge. |
After a shaky start in their early years, presbyopia-correcting intraocular lenses (IOLs) are starting to deliver more consistently on their promise of postoperative spectacle independence. Still, favored lens designs and surgical protocols differ greatly among surgeons. Wanting to establish a consensus on recommendations, researchers recently gathered 10 experts in the field to address such issues.
A steering committee sectioned 105 items into four sections (preoperative, intraoperative and postoperative considerations and IOL selection). Consensus among the experts was defined as ≥70% or seven of the experts agreeing with the evaluation of a statement.
Preoperative considerations included 68 items, and consensus was achieved in 70.6% (n=48). Consensus was reached in 10 out of the 14 intraoperative issues (71.9%) and in 10 out of the 13 postoperative considerations (76.9%).
Looking at preoperative considerations, age, patient habits, work type and motivation were all considered important when recommending a presbyopia-correcting IOL. Patients outside the range of 50 to 75 years old should be managed with more caution, and surgeons should weigh age against other preoperative considerations like refraction and ocular health, the researchers suggest. Visual requirements and suitability for an IOL are important takeaways from the patient’s profile, which also received consensus.
The experts agreed that the potential postoperative visual acuity is crucial in deciding the type of presbyopia-correcting IOL. They noted that patients with a potential post-op corrected distance visual acuity less than 0.5 (Snellen scale) should consider EDOF IOLs or non-diffractive IOL designs. Those expected to emerge post-op with greater than 0.5 may benefit from a multifocal IOL.
Recommending presbyopia-correcting IOLs achieved consensus in categories of refraction, keratometry and IOL power, but axial length saw discrepancy among the panel. Keratometry between 40D to 45D and IOL power between 10D to 27D were considered most suitable for a presbyopia-correcting lens; outside these ranges, patients should be managed with more caution. Both short and long eyes should be managed with more caution, indicated by IOL power consensus, as both present their own set of potential challenges with IOL implants.
Pupil size was also considered important, with both small and large pupils potentially causing more risks. Accordingly, the panel of experts agreed that an optimal range of pupil diameter for presbyopia-correcting IOLs is larger than 2.8mm under photopic conditions and smaller than 6.0mm under scotopic conditions.
Relative contraindications included dry eye disease, lid malposition, regular astigmatism greater than 5.0D, poor dilation, iris defect, synechiae and prior refractive corneal surgery (if corneal higher-order aberrations become problematic), among others. Absolute contraindications consisted of keratoconus, limbal stem cell deficiency, corneal epithelial or endothelial dysfunction, diabetic retinopathy and dry or wet AMD. Patients with age-related macular degeneration or a family history of such should receive recommendations of an EDOF IOL or one with a non-diffractive design.
Seven preoperative tests to reduce postoperative complications were agreed upon, including corneal topography and tomography, static pupillometry, biometry and biometry, OCT for retinal nerve fiber layer and macula assessment.
Finally, most experts agreed that IOL material for diffractive types should be hydrophobic or hydrophilic with a hydrophobic surface and that diffractive design is not necessary in presbyopia-correcting IOLs. However, parameters for choosing IOL characteristics received discrepancy, including material, platform and optic design. Consensus was only reached on the importance of patient habits for optic design selection.
Despite providing a solid baseline, the study authors caution that “this study was based on experts’ opinions, not evidence-based research. Consequently, the outcomes of this survey should be considered a guide. These recommendations only relate to a snapshot in time and may change as future tests and IOL designs become available.”
Romano V, Madrid-Costa D, Alfonso JF, et al. Recommendation for presbyopia-correcting intraocular lenses: a Delphi consensus statement by the ESASO study group. Am J Ophthalmol. May 24, 2023. [Epub ahead of print]. |


