 |
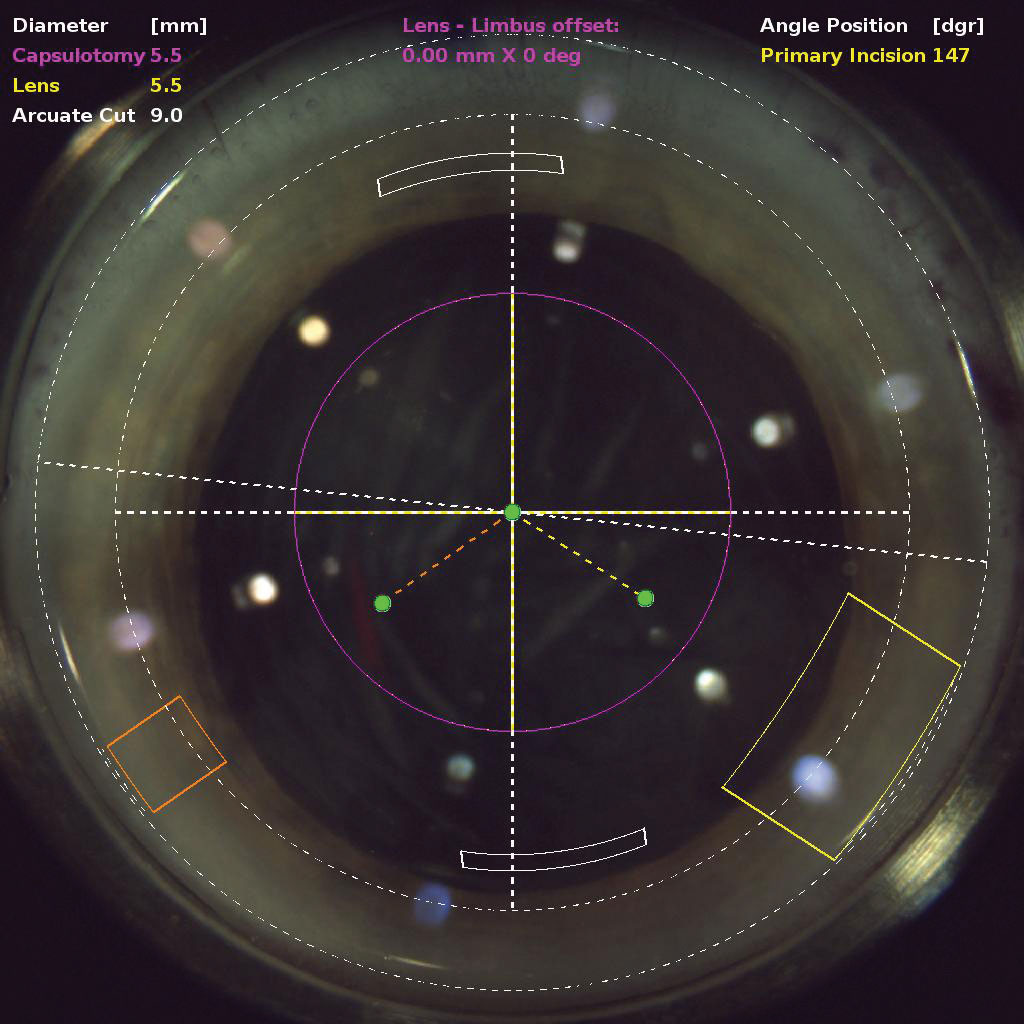
FLACS may be a better choice than conventional phaco for patients with hard cataracts, study finds. Photo: Justin Schweitzer, OD. Click image to enlarge. |
Score one for FLACS. The high-tech approach to cataract surgery, which replaces some manual steps with cuts made by a femtosecond laser, is a technical marvel but a tough sell. The American Academy of Ophthalmology recently concluded that FLACS is no safer or better than conventional phaco, but a new study finds value in the approach for some eyes that have undergone pars plana vitrectomy (PPV). Such cases pose additional challenges during cataract surgery for various reasons, such as fluctuating anterior chamber depth, weakened zonules and loss of vitreous support.
A recent study investigated how visual outcomes and complications of FLACS compare with those of conventional phacoemulsification in vitrectomized eyes. It found that FLACS may improve the safety of the procedure and shorten the period of visual rehabilitation, particularly in patients with hard nuclear cataracts.
The prospective controlled cohort study analyzed 86 eyes with cataracts and a nucleus grade between three and six post-PPV. The eyes, 43 of which had hard nuclei (grade five or six), were randomized to receive either FLACS (n=41) or conventional phacoemulsification (n=41). Prior to cataract surgery and at various time points throughout the three months post-op, the researchers recorded the following measurements: endothelial cell density, central corneal thickness and corrected distance visual acuity. They also analyzed intraoperative parameters as well as intra- and post-op complications.
Among FLACS patients with hard nuclei, the researchers noted that cumulative dissipated energy was significantly lower and ultrasound time was shorter. No differences in corrected distance visual acuity were observed between patients receiving either type of procedure.
Throughout the follow-up period, endothelial cell density decreased in both groups but especially in those with hard nuclei who received conventional phacoemulsification. Central corneal thickness returned to preoperative levels at three months post-op in both groups, but notably, eyes with hard cataract in the FLACS group had a quicker recovery. Only minor complications occurred during or after the procedure for both types of surgery.
An important observation from the study was the influence of residual emulsified SO
droplets in the anterior chamber on outcomes of FLACS, as well as the influence of preoperative pupil size. In their paper for Journal of Cataract and Refractive Surgery, the researchers noted that two of the three cases of incomplete capsulotomy in the FLACS group were “due to residual emulsified SO droplets blocking the laser from penetrating during capsulotomy, and one case was due to the pupil diameter not being sufficiently large during capsulotomy.” These cases were managed by manual supplemental capsulorhexis after staining the anterior lens capsule with 0.5% indocyanine green. Patients with either of these characteristics—residual emulsified SO droplets in the anterior chamber or an undilatable pupil—are not recommended as candidates for FLACS, they wrote.
“It would be better to transform to conventional phacoemulsification if the pupil diameter is smaller than 6.5mm, especially in patients with hard cataracts who intend to undergo FLACS,” the researchers noted. “In manual capsulorhexis, pupil dilation using intracameral mydriatics, iris hooks or the use of pupil expansion devices is successful in most patients.”
In conclusion, FLACS and conventional phacoemulsification can both produce good visual and clinical outcomes in patients with prior PPV. The former may quicken visual rehabilitation in patients with hard nuclear cataracts as long as they don’t have either of the contraindications mentioned above.
Cai L, Ma D, Xu X, et al. A comparative study of femtosecond laser-assisted cataract surgery versus conventional phacoemulsification for complex cataracts in vitrectomized eyes. J Cat Refract Surg. 2022. [Epub ahead of print]. |


