 |
|
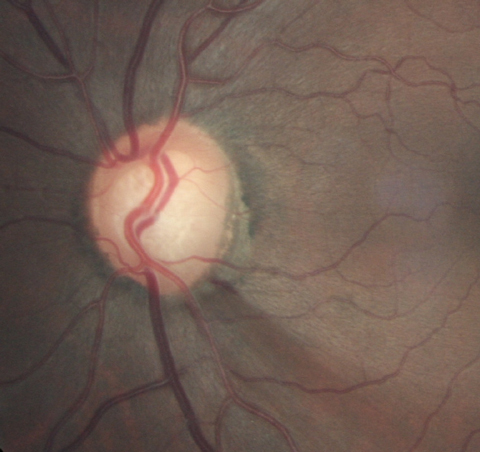
More focus should be put on implementing more frequent screening programs for glaucoma, especially since signs of the disease may present before its onset. Photo: Joseph Sowka, OD. Click image to enlarge. |
With glaucoma being one of the most common causes of blindness worldwide, doctors and patients alike would benefit from more robust screening efforts to potentially allow intervention before the disease manifests clinically, at which point irreversible damage has already occurred. An earlier trial demonstrated a 50% reduction of glaucoma-related blindness in a population that was routinely screened. A new study in JAMA Ophthalmology looked to expand on this by identifying the “preclinical detectable phase” (PCDP) of open-angle glaucoma, a component essential for planning and early evaluation of screening programs; the concept has been proven valuable in cancer screening.
The researchers conducted a retrospective medical record review of a large population-based screening for glaucoma conducted on 32,918 individuals, which yielded 2,029 glaucoma patients. The team then assessed new case prevalence at screening time and the expected clinical incidence, which is the number of new glaucoma cases that could be anticipated without screening. Main findings included a mean age of screening at 67.4 years and a mean PCDP length of 10.7 years for the entire study population, while the prevalence/incidence method yielded a mean PCDP of 10.1 years.
Glaucoma Screening Criteria UsedPatients with at least one of the following were considered positive:
|
The authors explain that “estimates of the length of the PCDP are important for early estimation of the expected effectiveness of screening, for decisions regarding optimum screening intervals, and for estimation of the amount of overdiagnosis.”1
They further elaborate that a shorter PCDP would indicate more rapid disease development into clinical stages, thus more frequent screening would be necessary to achieve the same effect. Seen here, though, is a longer PCDP, meaning only relatively infrequent screening would be necessary, about once every five years, the authors conclude. They also explain that an optimum interval between repeated screenings depends on age, sensitivity to screening, disease severity of interval cases and the mean PCDP.
With the practical application of this screening type still undecided, the authors note that “we have not tried to analyze whether screening is cost-effective, but our results suggest that screening for open angle glaucoma, if repeated, could be done with relatively long intervals.”1
The study conducted used data from a very specific cohort: an all-white Swedish population. This is one point that is emphasized by an invited commentator on the article, who points out that the age-dependent time course of open angle glaucoma will vary for other ethnic and racial groups.
As well, almost 80% of the general population invited for screening in the study participated and, of those, all received care at one institution. The author of the commentary notes that this rate of adherence would not be expected in most cultures and that the comprehensive examinations given are not routine for eye care.
Despite its potentially limited generalization, the commentator still believes that “this is a helpful initial insight for our considering the value, frequency, content and appropriateness of using sophisticated approaches to screen for POAG.”2
Both authors of the original study and the commentary see usage of this early development as beneficial. The commentator simply adds that “similar data are needed on other populations, which will vary with the efficacy and use of routine, comprehensive eye care services […] the ethnic and racial incidence and course of POAG in those populations, their adherence to recommended screening programs and the cost and accuracy of such sophisticated screening in the local context.”2
1. Aspberg J, Heijl A, Bengtsson B. Estimating the length of the preclinical detectable phase for open-angle glaucoma. JAMA Ophthalmol. November 23, 2022. [Epub ahead of print]. 2. Sommer A. Screening for primary open-angle glaucoma. JAMA Ophthalmol. November 23, 2022. [Epub ahead of print]. |


