The aim of a new study was to explore factors affecting the progression of neovascular age-related macular degeneration (nAMD) and identify predictive factors that can estimate the duration of intravitreal treatments. The Finnish researchers found that heavy smoking and high BMI are accelerating factors for earlier emergence of nAMD, while the presence of intraretinal fluid (IRF) is associated with rapid progression.
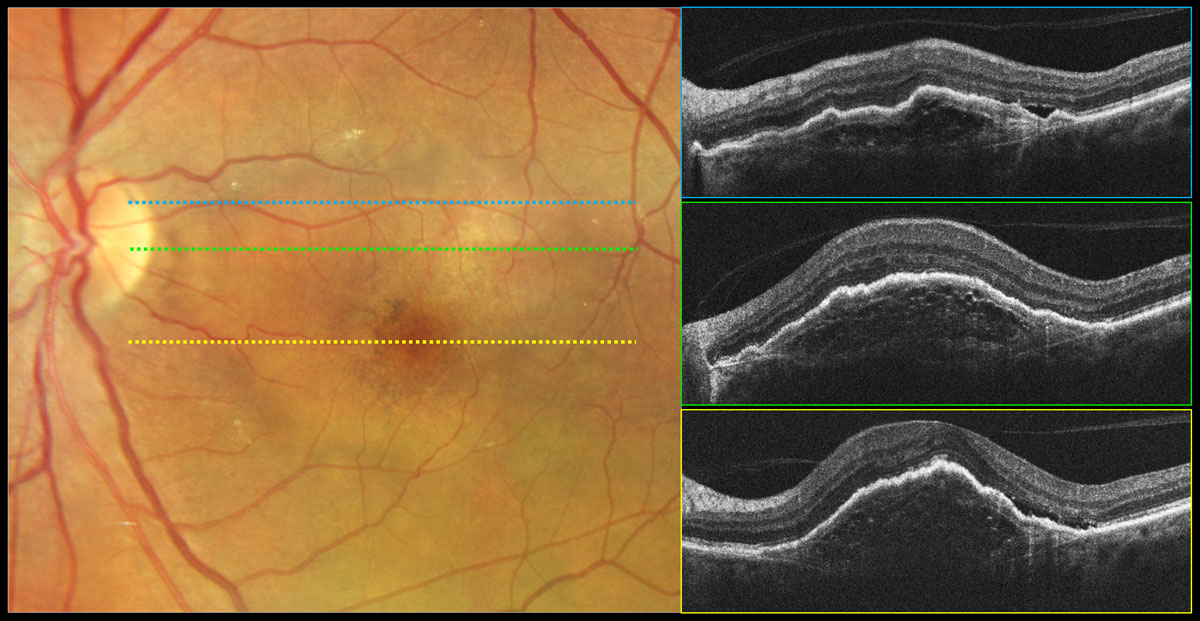 |
| The use of anticoagulants allowed wet AMD patients to remain on anti-VEGF treatment for a longer time, possibly due to their overall greater diligence with medication adherence. Photo: Carolyn Majcher, OD. Click image to enlarge. |
This retrospective study included 421 nAMD patients treated at the Kuopio University Hospital in Finland between 2007 and 2021. The collected data included background demographics, treatment history, visual acuity and retinal biomarker analysis. Impact of baseline factors on age at diagnosis, treatment duration, received treatment intensity and visual acuity gains were analyzed.
Heavy smoking and high body mass index (BMI) were associated with an earlier onset, while the use of anticoagulation and anti-aggregation medication were associated with a later onset of nAMD.
A low number of injections during the first year of treatment and the presence of IRF at baseline were associated with shorter treatment duration. “Interestingly, when IRF-only patients were compared to subretinal fluid (SRF)-only patients, IRF patients showed higher occurrences of subretinal drusenoid deposits,” the authors noted in their paper on the research. “In addition, when all patients with IRF were compared to SRF only patients, more hyperreflective foci (HRF) and complete RPE and outer retinal atrophy were observed in patients with IRF.”
Only patients who used anticoagulation drug and those who had only SRF on baseline remained on treatment for a longer period of time compared to the other patients. On the other hand, a low number of intravitreal anti-VEGF injections during the first year of treatment and the presence of baseline IRF were associated with a shorter treatment duration.
“In the short-treatment duration group, patients seemed to be less responsive to treatment and experienced faster vision decline, but also experienced fewer deaths. Therefore, we think that the faster dropout from the treatment in the short-treatment duration group was due to vision decline,” they wrote. On the other hand, patients using an anticoagulant maintained better vision during the first two years but had higher levels of anti-VEGF discontinuation due to death than those without anticoagulant use. “Thus, anticoagulation medication users may be more committed to treatment or respond better to the treatment regardless of their worse baseline general health.”
It should be noted that patients with only SRF at baseline were younger and had better baseline VA than patients with only IRF at baseline. Patients with only IRF at baseline died numerically more often during the anti-VEGF treatment, but the difference was not statistically significant. As patients with only IRF at baseline were older and had worse VA at baseline, we consider that their anti-VEGF treatments had been discontinued due to previously mentioned guidelines.
The authors observed that IRF was associated with an increased number of HRF, SDDs as well as a more severe atrophy level. “These factors are considered to be associated with disease progression or worse prognosis for a patient. Thus, their enrichment in the IRF-positive population is fascinating especially as we had observed IRF to be linked with faster progression of nAMD,” the authors noted.
These findings reveal that even though cardiovascular diseases can increase the risk of nAMD, proper medication of these diseases and thus better vascular health could be able to delay the onset of nAMD.
“Curiously, all our findings can be linked to the health of vasculature and thus our results underline the importance of keeping in mind the potential role of disturbed vasculature function during the whole disease course of nAMD,” the authors concluded. “Our results may help ophthalmologists judge an individual's risk for disease progression and may draw more attention to early lifestyle intervention to delay nAMD onset as well as help identify patients who are at risk for fast disease progression.”
Helotera H, Siintamo L, Kivinen N, et al. Analysis of prognostic and predictive factors in neovascular age-related macular degeneration Kuopio cohort. Acta Ophthalmologica. March 13, 2024. [Epub ahead of print.] |


