 |
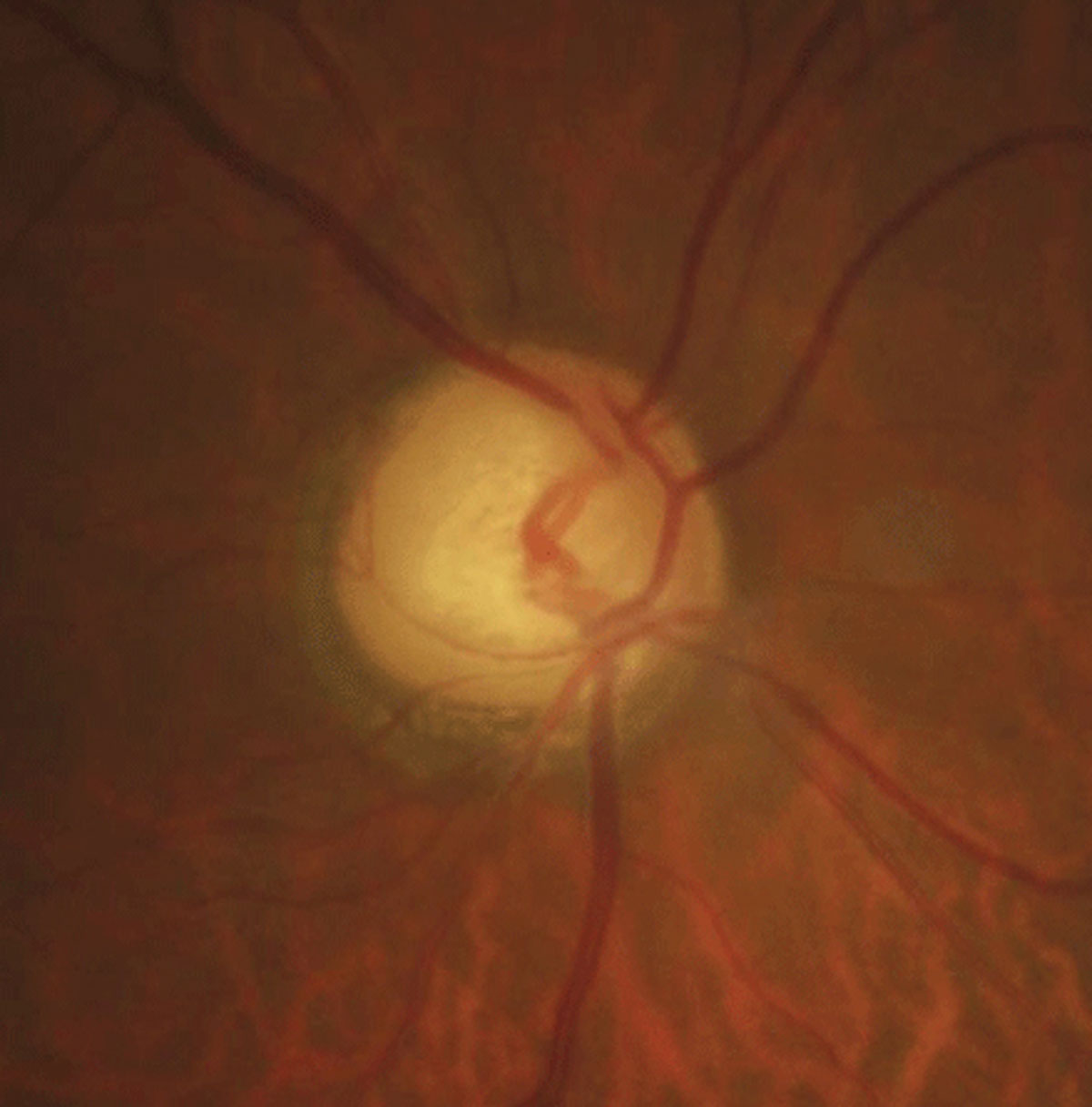
There was a significant positive correlation between BMI percentile and Goldmann-correlated IOP, as well as with corneal hysteresis and corneal resistance factor values. Photo: Justin Cole, OD, and Jarett Mazzarella, OD. Click image to enlarge. |
Despite the well-established association of obesity with ocular conditions like ocular hypertension/glaucoma, premature cataract and age-related maculopathy, its impact on corneal biomechanics and IOP values remains less explored, especially in pediatric populations. By addressing these research gaps, researchers can gain valuable insights into the relationship between obesity and ocular parameters, ultimately contributing to the enhanced understanding and management of obesity-related ocular conditions in pediatric patients.
In a recent study published in Journal of Glaucoma, a team in Turkey investigated the effect of obesity on corneal biomechanics as measured by Ocular Response Analyzer (ORA; Reichert), retinal nerve fiber (RNFL) layer and central macular thickness in children. They found that higher Goldmann-correlated IOP, corneal hysteresis and corneal resistance factor values suggest that obese children could be potential candidates for glaucoma.
This prospective, cross-sectional, comparative study evaluated 146 eyes of normal-weight, overweight and obese children between the ages of six and 17 (43 boys and 30 girls). Mean age among the three groups was 12.5, 13.2 and 13.5, respectively. BMI percentile was found to be 44.5%, 88.8% and 98.7%, respectively.
The findings revealed that the mean Goldmann-correlated IOP value was significantly higher in obese but not in overweight children; however, the mean corneal hysteresis and corneal resistance factor values are significantly higher not only in obese but also overweight children. There was no statistically significant difference regarding age, sex, corneal compensated IOP, average RNFL thickness, cup-to-disc ratio or central macular thickness among the groups.
The researchers suggest the possibility that “excess weight may alter the composition or structure of the cornea, leading to changes in its biomechanical properties.”
The team did note that the biometric characteristics of the study eyes, such as central corneal thickness and axial length measurements, were not taken into account, which may have influenced the study outcomes. “It is worth acknowledging that the duration of obesity could potentially impact corneal biomechanical properties and OCT findings; regrettably, this study lacks data regarding the duration of patients’ obesity,” they wrote in their paper.
The researchers believed that their study underscores the importance of regular IOP and retinal assessments for early detection and management. “The significant elevation in corneal hysteresis and corneal resistance factor values observed in overweight children compared with those of normal weight implies that corneal biomechanics may be one of the parameters to be considered in the diagnosis and follow-up of these children,” they concluded. “We hope that the findings obtained from this preliminary study will provide a valuable contribution to future research endeavors aimed at enhancing our comprehension of the interplay between corneal biomechanics, retinal structures and childhood obesity.”
Eroglu SA, Unsal AIA, Verdi F, et al. The effect of childhood obesity on intraocular pressure, corneal biomechanics, retinal nerve fiber layer and central macular thickness. J Glaucoma. March 19, 2024. [Epub ahead of print]. |


