 |
|
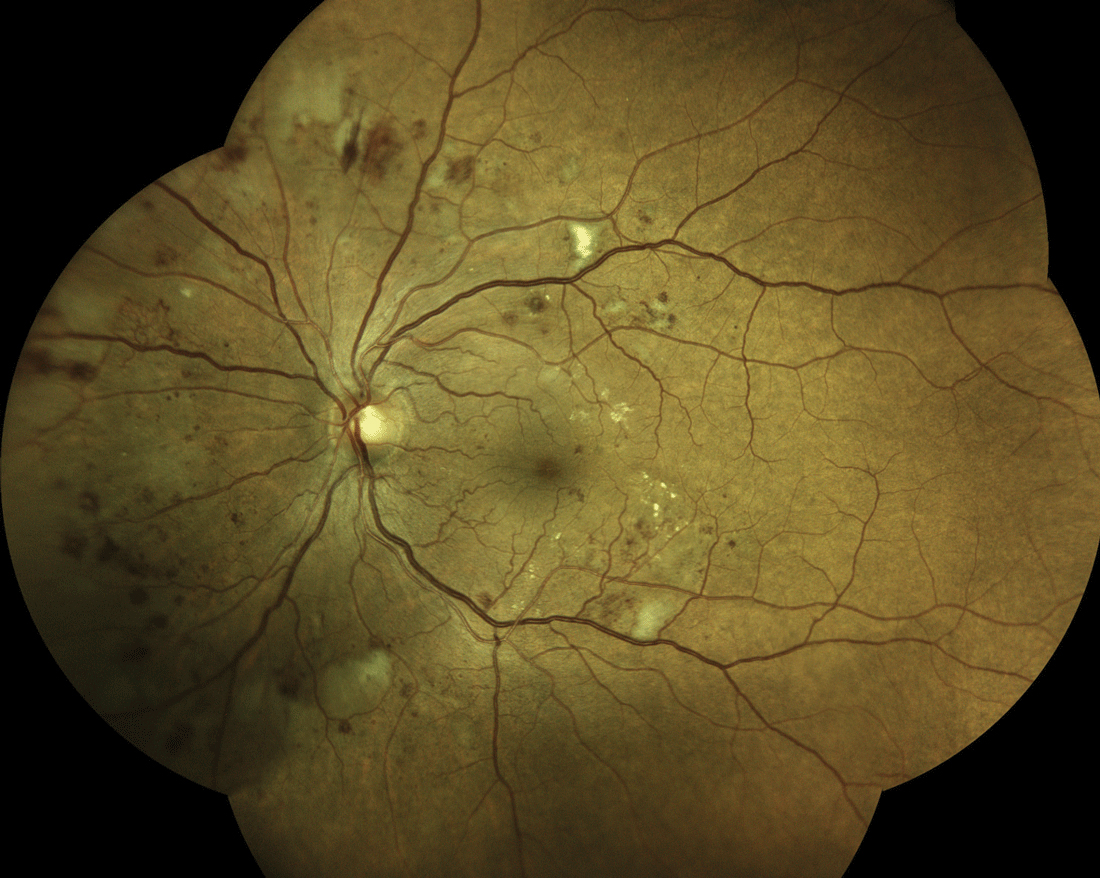
Data analysis models for proliferative DR demonstrated acceptable predictive ability in a healthcare system. Photo: Steven Ferrucci, OD. Click image to enlarge. |
There have been improvements in screening, diagnosis and treatment for diabetes and diabetic retinopathy (DR) since many of the studies that identified disease risk factors were first conducted, and many researchers believe that the risk factors for progression should be revisited. A study based out of the University of California, San Francisco (UCSF), developed survival models for predicting progression from nonproliferative to proliferative DR using variables at different timepoints and evaluated the model using EHR data from two different health systems. Insurance status was selected by all four models indicating high predictive ability. However, updating the baseline variables with new clinical information from within six-month follow-up did not consistently improve the predictive performance.
The study, published in Ophthalmology Science, used data from UCSF and Zuckerberg San Francisco General (ZSFG) to identify patients with a diagnosis of nonproliferative DR, age ≥18 years, a diagnosis of type 1 or 2 diabetes mellitus, ≥six months of follow-up and no prior diagnosis of proliferative DR before the index date (date of first nonproliferative DR diagnosis in the EHR). Four survival models were developed: Cox proportional hazards, Cox with backward selection, Cox with LASSO regression and Random Survival Forest. For each model, three variable sets were compared to determine the impact of including updated clinical information: Static0 (data up to the index date), Static6m (data updated six months after the index date) and Dynamic (data in Static0 plus data change during the six-month period).
The UCSF cohort included 1,130 patients, and 8.1% of patients progressed to proliferative DR. The ZSFG cohort included 687 patients, and 4.4% of patients progressed to proliferative DR. All models performed similarly in internal validation. The Random Survival Forest with Static6m set performed best in external validation. Insurance and age were selected or ranked as highly important by all models. “While insurance status has not been specifically identified as a risk factor of progression, other studies investigating different aspects of diabetic retinopathy care have found insurance-based disparities to be a key risk factor in outcomes,” the study authors noted in their paper.
Patients with more previous strokes or hospital admissions were also at a greater risk of progression to proliferative DR. The researchers were led to believe that these findings indicate that the microvascular pathology of DR may have larger macrovascular implications, which need to be further explored. The models also confirmed other known predictors that were important for progression, including younger age, greater nonproliferative DR severity, presence of neuropathy and higher HbA1c.
The study did point out that, due to the likely incompleteness of EHR data and the fact that it did not include a look-back period before the index date to avoid decreasing sample size, the first nonproliferative DR diagnosis does not represent incident DR.
“Future directions include additional corroboration at other medical centers, as well as further investigation into the clinical relevance of these novel predictors,” the researchers concluded.
Guo Y, Yonamine S, Ma CJ, et al. Developing and validating models to predict progression to proliferative diabetic retinopathy. Ophthalmol Sci. January 31, 2023. [Epub ahead of print]. |


