 |
|
A moving stimuli may help improve glaucoma diagnosis from VF testing. Photo: Danica Marrelli, OD. Click image to enlarge. |
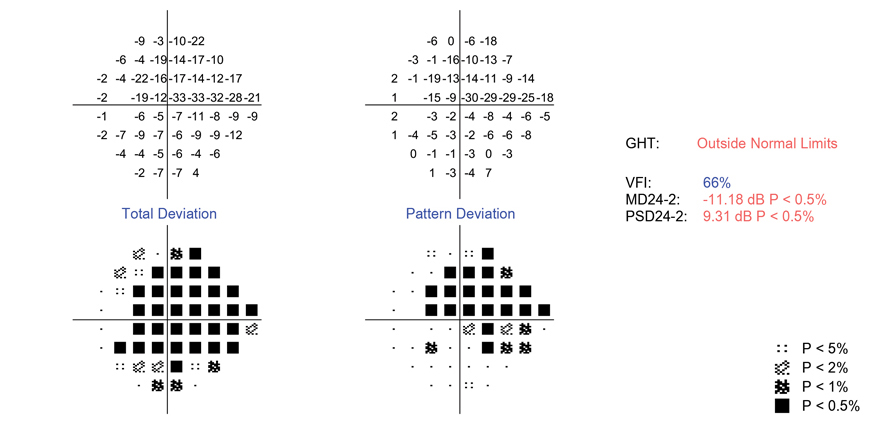
It is important to develop new perimetric techniques that can reliably and accurately assess functional progression in regions of moderate and severe glaucomatous loss. Current stimulus detection remains probabilistic rather than deterministic, so estimates of sensitivity are too variable to be considered reliable at this level of disease. Researchers recently introduced an alternative approach to further extend the dynamic range of perimetry: increasing sensitivity by introducing motion. They believe that moving stimuli may be easier to detect than static stimuli of the same contrast. The team anticipates an even greater effect in regions damaged by glaucoma, where the primary limiting factor for sensitivity is the remaining number of healthy retinal ganglion cells, especially motion-sensitive retinal ganglion cells.
In their study, the researchers determined that using a moving stimulus instead of a static one, in an otherwise identical seen/not seen perimetric task similar to those used clinically, both extended the dynamic range into locations with more advanced disease and decreased test-retest variability within the dynamic range.
Testing was conducted on an Octopus (Haag-Streit) perimeter controlled by a custom-written program. A moving stimulus was designed to travel parallel to the average nerve fiber bundle orientation at each location and compared against an otherwise identical static stimulus. To assess dynamic range, psychometric functions were measured at four locations in 10 subjects. To evaluate clinically realistic test-retest variability, 34 locations of 94 glaucoma patients and suspects were tested twice, six months apart.
Using static stimuli, nine of the 40 psychometric functions had less than a 90% maximum response probability, suggesting that they exist beyond the dynamic range. Eight of those locations had an asymptotic maximum of more than 90% with moving stimuli. Sensitivities were higher for moving stimuli; the difference increased as sensitivity decreased. Test-retest limits of agreement were narrower for moving stimuli (-6.35dB to +6.48dB) than static stimuli (-12.7dB to +7.81dB).
Most subjects in the study reported preferring testing with the moving stimulus. This preference strengthened, from 42% on the first visit to 62% on the second visit, suggesting that it was not purely due to the novelty of the test. The static stimulus resulted in wider interquartile ranges at most locations. By increasing the range of stimuli, this factor also increased the variability of stimulus presentations, creating uncertainty in the subject over whether they saw the stimulus. Subjective uncertainty can be stressful, causing patients to prefer the moving stimulus test instead.
“If defect detectability with the moving stimulus is equal to, or better than, with the static stimulus, then it would be reasonable to use a stimulus whose magnitude of movement is constant, as in the current study,” the researchers wrote in their paper.
The study suggested this test could eventually be implemented on current instruments, easing translatability of the findings and making any transition easier for patients.
“Given the known high variability of current perimetry especially in damaged areas, and the lack of other test modalities for monitoring disease progression in regions of advanced loss, we suggest that use of a moving stimulus may improve the diagnostic usefulness of functional testing for glaucoma,” the team concluded.
Gardiner SK, Mansberger SL. Moving stimulus perimetry: a new functional test for glaucoma. Transl Vis Sci Technol. 2022;11(10):9. |


