 |
|
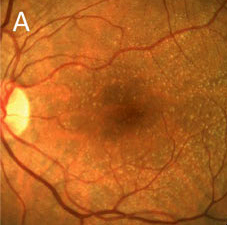
Early-stage AMD seems to be increasing in prevalence according to new data. Click image to enlarge. |
Editor’s Note: As part of our “Year in Review” retrospective, we’ve selected the top 30 news stories of the year and are re-sharing them as we close out 2022. Follow along as we count down to number 1!
This story was originally published on November 8, 2022.
No. 2 biggest news story of 2022:
Although age-related macular degeneration (AMD) is one of the top causes of vision loss and blindness, nationwide estimates of its impact have not been calculated in over a decade and early-stage AMD estimates of prevalence have been inconsistently measured, researchers say. One new study has aimed to fill in this gap, estimating prevalence of early- and late-stage AMD
The study estimated that 18.3 million people 40 years or older were living with early-stage AMD in 2019, for a prevalence rate within this age group of 11.6%. Late-stage AMD was estimated to have a prevalence of 0.9% or 1.5 million people over age 40.
The retrospective study, published in JAMA Ophthalmology, sourced its data from the American Community Survey, National Health and Nutrition Examination Survey US Centers for Medicare & Medicaid Services claims for fee-for-service beneficiaries and population-based studies. Studies included for analysis were recorded via data from the US Centers for Disease Control and Prevention’s Vision and Eye Health Surveillance System.
To determine between early- and late-stage AMD manifestations, the study defined early-stage AMD as retinal pigment epithelium abnormalities or the presence of drusen 125 or more microns in diameter in either eye, while late-stage was defined as choroidal neovascularization and/or geographic atrophy in either eye.
Both stages’ prevalence rates were found to vary by geography as well as demographics. Early-stage AMD rates standardized for age and sex were lower in non-Hispanic Black individuals than any other ethnicity group. Late-stage AMD rates standardized for sex and age were additionally lower for non-Hispanic Black individuals as well as Hispanics when compared with other ethnicities.
While the study’s estimated prevalence of late-stage AMD at 0.9% was comparable to prior studies’ estimations, their early-stage estimation was slightly higher than earlier projections made. The authors identify multiple reasons this may have been the case, such as the use of 2019 population data that includes a significant amount of more people in the oldest age groups. Another possibility could be due to the authors’ inclusion of a model that estimated increase in prevalence of those over 80 years old, while older estimations did not take an aging population into account.
The authors clearly highlight what this study adds to the current literature of AMD estimates that has not been done before. As they describe, the study’s “primary contributions of this work as compared with earlier estimates include updating US population demographics, the inclusion of individuals in group quarters, inclusion of newer population-based study data and estimation of state and county estimates.” These inclusions serve to provide more accurate, reflective numbers, and that these “state-level and county-level AMD estimates may help guide public health practice.”
Rein DB, Wittenborn JS, Burke-Conte Z, et al. Prevalence of age-related macular degeneration in the US in 2019. JAMA Ophthalmol. November 3, 2022. [Epub ahead of print]. |


