 |
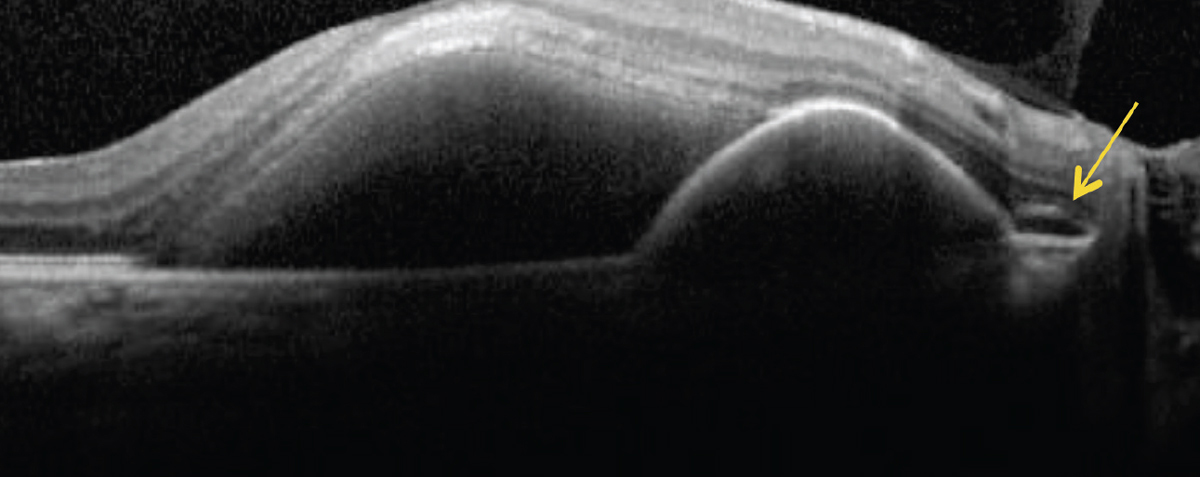
| Polypoidal lesions seen with PCV seem to regress more with combination intravitreal anti-VEGF and photodynamic therapies. Photo: Rim Makhlouf, OD. Click image to enlarge. |
New research from Munich sheds light on the emerging area of so-called “pachychoroid spectrum” diseases. Using OCT, the researchers evaluated the misdiagnosis rate of polypoidal choroidal vasculopathy (PCV) among those originally diagnosed with pachychoroid neovasculopathy (PNV).
A total of 49 eyes from 44 patients were included with a clinical PNV diagnosis. Of these, 85.7% had PNV, while 14.3% were determined to have misdiagnosed PCV. Subfoveal choroidal thickness was comparable in both groups, and there were no differences seen in total pigment epithelial detachment (PED) diameter. There was also no observed difference in age.
The team found maximum PED height to be higher in those with PCV. After analysis, the optimum cutoff to define “peaking PED” was 158μm. As well, subretinal hyperreflective material, subretinal ring-like structures and subretinal pigment epithelium fluid were all more prevalent in PCV eyes, with subretinal fluid present in 42.9% compared with 7.7% in PNV eyes and hyperreflective material present in 71.4% of PCV eyes compared with 28.6% of PNV eyes.
The study authors highlighted the cutoff value. Although recognizing that this is a simplified approach, they believe the 158μm marker could serve as a solid first indicator of PCV, especially when followed with more imaging, such as indocyanine green angiography.
Not only is this a way to provide greater distinction, but it also has prognostic implications. PCV is considered a more aggressive form of pachychoroid neovascularization. As one previous paper found, this form was more frequently associated than PNV with aggressive OCT biomarkers of disease, including intraretinal fluid (38.2% vs. 12.2%) and macular hemorrhage (51.4% vs. 12.2%).
As the authors explain in their paper for the journal Eye, higher incidence of macular hemorrhage seems to impact long-term prognosis, since vitreous breakthrough hemorrhage often results in needed pars plana vitrectomy. Consequently, PCV eyes receive more annual anti-VEGF injections, on average, than PNV eyes.
Observing data from the EVEREST II trial, they suggest that anti-VEGF/photodynamic combination therapy over anti-VEGF treatment alone may help to close polypoidal lesions in these patients, resulting in better visual acuity and reduced hemorrhage risk.
The authors emphasize the importance of establishing OCT criteria for two reasons: “Although most hospitals and private practices can readily offer OCT, fluorescein angiography is lacking in some, and indocyanine green angiography is unavailable in many clinical institutions. Second, OCT is by far the most widespread and recognized retinal imaging method, and clinicians nowadays seem to devote most of their time to the interpretation of OCT.”
Siedlecki J, Klaas J, Keidel L, et al. Optical coherence tomography-based misdiagnosis and morphological distinction in pachychoroid neovasculopathy vs. polypoidal choroidal vasculopathy. Eye. May 8, 2023. [Epub ahead of print]. |


