 |
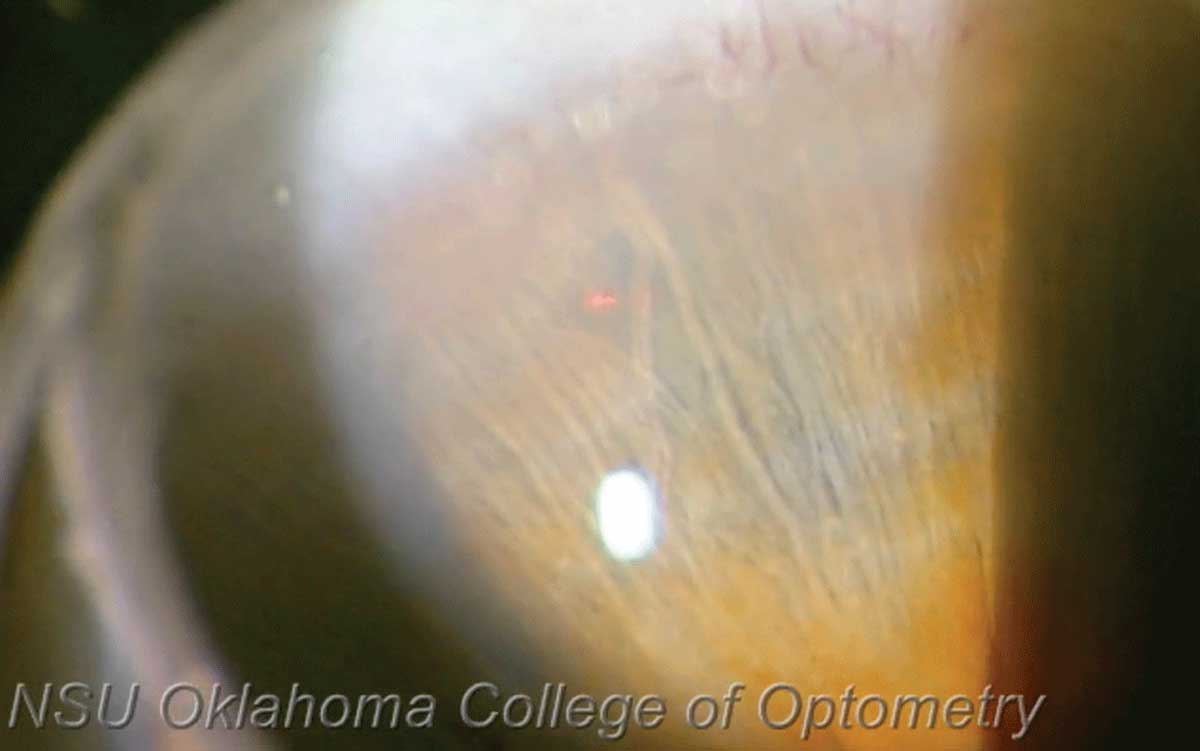
LPI may provide a solution for those at high risk of developing primary angle closure. Photo: Joseph Shetler O,D, and Nathan Lighthizer, OD. Click image to enlarge. |
A recent Chinese study assessed the value of preventative use of laser peripheral iridotomy (LPI) in at-risk patients who were followed for 14 years. Laser peripheral iridotomy (LPI) was performed on 889 patients aged 50 to 70 who were bilateral primary angle closure suspects (PACS). In the study, published last week in Ophthalmology, researchers wanted to identify risk factors for conversion from PACS to primary angle closure (PAC).
One LPI was performed at random to one eye in patients, with the fellow eye serving as the control. Outcomes were determined by PAC incidence, a composite endpoint including peripheral anterior synechiae, intraocular pressure (IOP) greater than 24mm Hg and acute angle closure.
During the 14 years, 390 treated eyes and 388 controls were lost to the follow-up, leaving 33 treated eyes and 105 controls that reached primary endpoints. Eyes treated with LPI displayed severer nuclear cataract, higher IOP, larger angle width and limbal anterior chamber depth than control eyes at the 14-year follow-up.
Developing endpoints was associated with higher IOP, shallower limbal anterior chamber depth and central anterior chamber depth in control eyes. Similarly, treated eyes were more likely to develop PAC if they displayed higher IOP, shallower limbal anterior chamber depth, or less IOP elevation after dark room-prone provocative tests.
PAC development risk was fairly low in the PACS population over the 14 years, and an approximate two-thirds (69%) decrease in PAC incidence occurred for eyes treated with LPI. The authors note that this difference was owed to an almost threefold higher incidence of peripheral anterior synechiae in control eyes.
Even further, the safety of LPI was corroborated by the similar visual acuities found between treated and non-treated eyes. Although treated eyes did show a higher degree of nuclear cataract, only 16 additional cataract surgeries for the 889 patients were needed in the 14 years.
Based on these results, the authors suggest that “prophylactic LPI should be preferentially recommended to those at highest risk of angle closure because the annual incidence of PAC was low and acute angle closure/PAC glaucoma were relatively rare in the community-based PACS population over the long-term.”
However, of the eyes that did convert to PAC, the mild peripheral anterior synechiae observed indicates a benign disorder, with only 2% to 6% of these eyes progressing to PAC glaucoma every year. Laser or cataract surgery on these eyes mostly resulted in stability that were diagnosed within the first six years, and only four control eyes developed into PAC glaucoma until the 14-year visit.
Finally, the authors attributed limbal anterior chamber depth and central anterior chamber depth as risk factors for rapid PACS progression, based on their findings. The slightly increased IOP seen in treated eyes they contend is likely due to postoperative inflammation responses and dynamic changes to the aqueous humor outflow.
The authors concluded that “although baseline IOP, IOP change after dark room-prone provocative tests, limbal anterior chamber depth and central anterior chamber depth were significantly associated with PAC occurrence in LPI-treated or control eyes, more potent predictors are still needed to realize precise prediction and guide targeted intervention in the future.”
Yuan Y, Wang W, Xiong R, et al. 14-year outcome of angle-closure prevention with laser iridotomy in the Zhongshan Angle Closure Prevention Study: extended follow-up of a randomized controlled trial. Ophthalmology. April 6, 2023. [Epub ahead of print]. |


