 |
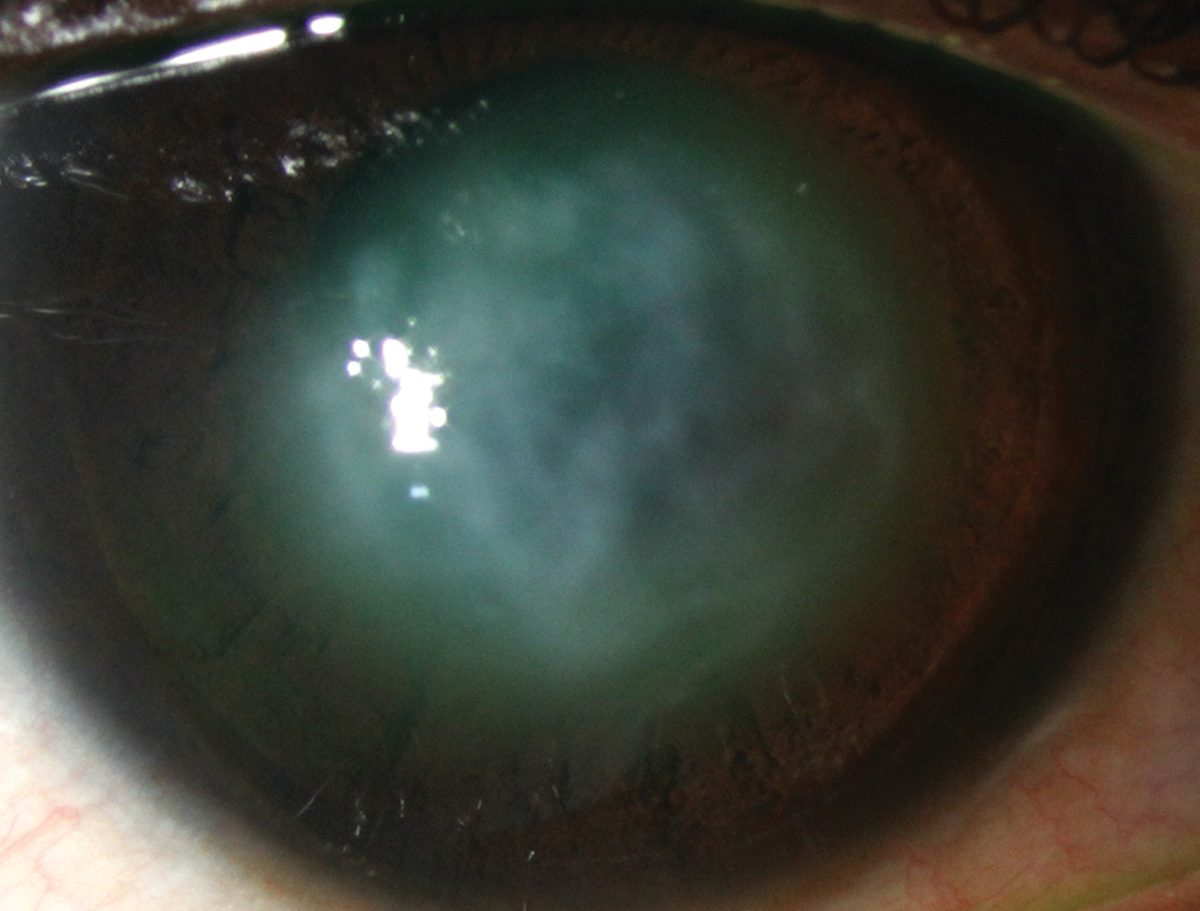
| Despite the challenges of obtaining data through edematous corneas, the researchers still recommend routine corneal tomography to assess changes over time in eyes after hydrops. Photo: Alison Bozung, OD. Click image to enlarge. |
As if keratoconus wasn’t bad enough, some patients develop the serious complication of acute corneal hydrops, where Descemet’s membrane ruptures and allows aqueous inflow into the cornea. Stromal edema and corneal opacification follow. Fortunately, this complication isn’t common, but experts note that its risk factors are poorly understood. To gain better understanding, researchers assessed clinical and tomographic factors that predispose keratoconus patients to this complication and found that steep keratometry, thin corneas and Down syndrome may be risk factors.
The retrospective study included patients seen at a single institution between 2015 and 2023 with advanced keratoconus (controls) and those that developed acute corneal hydrops. In total, 23 eyes of 19 patients developed acute corneal hydrops during the follow-up period. The researchers reported that the hydrops group and control group had similar incidence of known clinical associations, such as seasonal allergies, eye rubbing, snoring, asthma and eczema. The hydrops group had a higher incidence of Down syndrome.
The researchers also reported that despite similar best-corrected visual acuity on initial examination, the hydrops eyes had steeper keratometry values and thinner corneas than controls at baseline. They noted that right after hydrops development, there was “expected decline in visual acuity in the setting of corneal edema.” As the corneal edema resolved, these patients demonstrated progressive corneal flattening and reduced maximum keratometry over time. The hydrops group showed significant reduction in maximum keratometry at the final follow-up visit.
“While corneal flattening would be expected to be associated with improved vision, unfortunately, best-corrected visual acuity remained markedly poor compared with controls on final examination,” the researchers wrote in their Cornea paper. The final best-corrected visual acuity was worse than at baseline before hydrops development and worse compared with control eyes. Ultimately, 12 of 21 hydrops eyes underwent penetrating keratoplasty.
The researchers concluded that steep keratometry and thin corneas predispose keratoconus patients to acute corneal hydrops, but only having Down syndrome was significant. “It’s been difficult to distinguish these [clinical risk] factors from general risk factors of keratoconus progression,” they wrote.
As to why only Down syndrome was found to be significant, they suggested that “this may be because of more aggressive eye rubbing habits with Down syndrome. In fact, patients with Down syndrome have higher likelihood of developing bilateral acute corneal hydrops with chronic recurrent corneal edema.”
Yu SN, Gad R, Kutler R, et al. Scheimpflug-based tomographic risk factors for the development of acute corneal hydrops in keratoconus. Cornea 2024;00:1-4. |


